11th March 2024, NIA Diagnostic Imaging
It is actually not that difficult to diagnose pulmonary embolism. Patients with chest pains, shortness of breath, tachycardia and perhaps, light headedness might suggest pulmonary embolism. However, on their own, those symptoms may be from a number of medical conditions. Only with a high index of suspicion would you consider ordering more investigations looking for pulmonary emboli. Naturally, early diagnosis is vital. CT Pulmonary Angiogram (CTPA) is the key to diagnosing a Pulmonary Embolism.
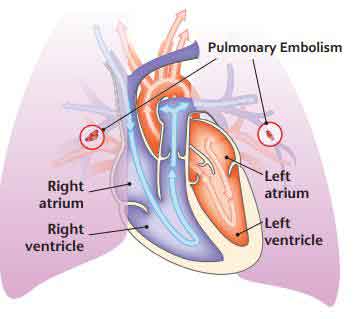
Pulmonary emboli (PE) arises when the blood flow in the pulmonary artery or its branches is disturbed by a thrombus originally occurring elsewhere in the body. Commonly, PE will occur after a deep vein thrombosis (DVT) has occurred within the deep veins, usually in the lower limbs. A thrombus which has developed is susceptible to break off, in which a part of the thrombus may migrate into pulmonary circulation. Whilst rare, PE may occur due to embolisation of air, fat or tumour cells which have migrated into pulmonary circulation. (2)
In the body, all veins drain into larger veins which carry blood to the right side of the heart and into the pulmonary arteries. As such, this embolus will migrate to the right side of the heart through the venous system, entering the pulmonary artery. Moreover, if there are multiple clots, they can progress into one or both lungs in different areas (3). Usually, pulmonary emboli are multiple and more commonly occur in the lower lobes of the lungs (2). Hence, a PE is a medical emergency as the blockage prevents normal blood flow and gas exchange leading to reduced oxygen levels in the body, stressing and damaging organs such as the brain, kidneys and heart (3).
Symptoms of Pulmonary Embolism may include:
• Shortness of Breath especially on exertion
• Sudden onset of sharp chest pain
• Difficulty breathing
• Light headedness
• Dizziness
• Rapid Heart rate
• Haemoptysis
What is a CT Pulmonary Angiogram (CTPA)?
Multi-detector CT pulmonary angiography is the imaging modality of choice for the diagnosis of queried pulmonary embolism (PE) due to its high sensitivity and specificity. As a result of high morbidity and mortality rates it is essential that patients are diagnosed promptly. The scan involves using a bolus-tracking technique whereby iodinated contrast agent paired with a
saline chaser is injected through a vein using a 20G cannula, using a minimum flow rate of 4.5mls/s (5).
A monitoring slice is taken below the carina at the level of the pulmonary trunk, where a ROI is then place on the pulmonary artery. In this selected region, sequential axial slices are conducted whilst the injection of contrast occurs until enhancement reaches 150 HU which will immediately trigger the scan. The acquired scan range will be from apices to the costophrenic angle (4).

CTPA is performed using a shallow inspiratory breath hold, to reduce the Valsalva manoeuvre occurring with deep breath hold as it may lead to poor vascular opacification due to the contrast bolus being diluted with unopacified blood flowing from the IVC (6).
At NIA Diagnostic imaging, with our latest CT technologies we are able to diagnose PE quickly through multiplanar reconstruction techniques, maximum intensity projections (MIPs), multi planar reformation (MPR) and volume rendering (VR) (5).
Radiographic features suggestive of PE:
Acute pulmonary emboli will result in an intraluminal filling defect within the pulmonary vasculature on a CT pulmonary angiogram. They form a sharp interface with the iodinated contrast medium. Acute pulmonary emboli may completely occlude the vessel with the entire lumen not being opacified, the vessel may enlarge, a central filling defect may occur where IV contrast surrounds the emboli or a peripheral intraluminal filling defect may occur that makes an acute angle with the vessel wall (7).
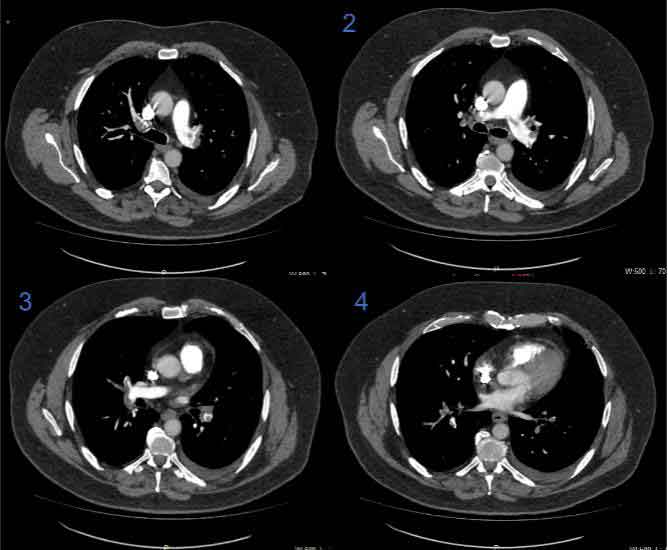
(RADIOGRAPHING APPEARANCE: Above axial images sequentially showing extensive, bilateral pulmonary emboli in patient with clinical history of shortness of breath on exertion and sharp chest pain)
Contraindications:
CTPA scans are contraindicated in patients who have renal insufficiency (eGFR <30) or patients who have moderate to severe allergy to iodinated contrast. Evidently, due to the urgent nature of PE diagnosis, the risk of the contraindications must be weighed up against the clinical urgency of performing the scan. Alternative imaging modalities such as V/Q scans or premedication may be considered for patients who are allergic to iodine and intravenous pre hydration may be considered for renal insufficiency (2).
Conclusion
At NIA Diagnostic Imaging, we understand the importance of early diagnosis of PE and accept all urgent requests for CTPA examinations. All Medicare eligible examinations are bulk billed under Medicare, including CTPA scans. With having highly experienced radiographers and radiologists on site, CT services are readily accessible at all NIA Diagnostic Imaging clinics. Please contact us for any further information: NIA Glenquarie Radiology (02) 9158 8660 info@niaimaging.com.au NIA Ingleburn Radiology (02) 8104 0803 info.ingleburn@niaimaging.com.au
References:
1. Thrombosis and Haemostasis society of Australia and New Zealand (n.d.). Pulmonary Embolism: PE. Accessed 06 Mar 2024. https://www.thanz.org.au/documents/item/359#:~:text=A%20Pulmonary%20Embolism%20(PE)%20is,and%20stopped%20in%20the%20lungs.
2. Vyas V, Goyal A. Acute Pulmonary Embolism. 2022, StatPearls Publishing, viewed 06 Mar 2024 https://www.ncbi.nlm.nih.gov/books/NBK560551/
3. American Thoracic Society, Patient Education Series – Pulmonary Embolism (n.d.) Accessed 06 Mar 2024. https://www.thoracic.org/patients/patient-resources/resources/pulmonary-embolism.pdf
4. Murphy, A. (n.d.). CT pulmonary angiogram (protocol) | Radiology Reference Article | Radiopaedia.org. Radiopaedia. https://radiopaedia.org/articles/ct-pulmonary-angiogram-protocol
5. Liu, D., Cai, X., Che, X., Ma, Y., Fu, Y., & Li, L. (2020). Visibility and image quality of peripheral pulmonary arteries in pulmonary embolism patients using free-breathing combined with a high-threshold bolus-triggering technique in CT pulmonary angiography. The Journal of international medical research, 48(8), 300060520939326. https://doi.org/10.1177/0300060520939326
6. Bhalla, A. S., Das, A., Naranje, P., Irodi, A., Raj, V., & Goyal, A. (2019). Imaging protocols for CT chest: A recommendation. The Indian journal of radiology & imaging, 29(3), 236–246.https://doi.org/10.4103/ijri.IJRI_34_19
7. Wittram, C., (2007), How I Do It: CT Pulmonary Angiography. American Journal of Roentgenology, Volume 188, Issue 5. https://doi.org/10.2214/AJR.06.1104
