8th September 2024, NIA Diagnostic Imaging

Computed tomography (CT) is widely recognised as the gold standard for detecting and diagnosing a broad range of pathologies due to its ability to provide detailed cross-sectional imaging. However, concerns about radiation exposure continue to be raised by both patients and clinicians. As a result, it is crucial to understand the impact of technological advancements in ensuring that radiation exposure is kept as low as reasonably achievable (ALARA) while still maintaining diagnostic accuracy. Evaluating the risks and benefits of radiation during CT examinations is key to making informed choices and maintaining patient safety, satisfaction, and care.
HOW DOES RADIATION CAUSE CANCER?
The radiation produced by x-ray and CT is ionising radiation, which are high-energy wavelengths that permeate the tissue to reveal the body’s internal organs and structures. Ionising radiation can damage the body’s DNA, and while our cells are capable of mending the majority of the damage, occasionally there may be minor errors in the repair. As a result, DNA mutations may occur, which could eventually lead to cancer (3).
RADIATION DOSE AND RISKS ASSOCIATED WITH CT SCANS
The radiation dose from a CT scan varies for each patient and is influenced by factors such as age, gender, the size of the body part being examined, the type of scan, and the specific CT equipment and settings used (9).
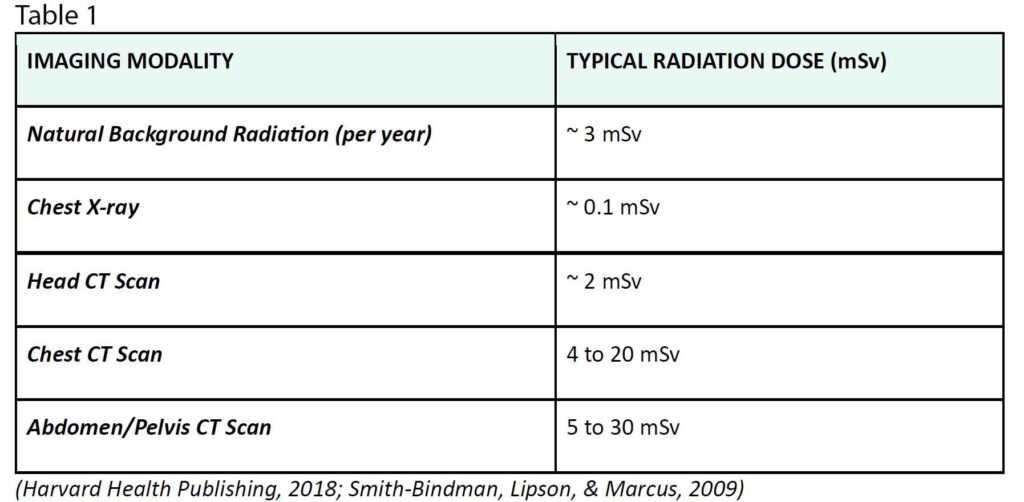
The table below compares the average radiation doses for head CT scans, abdominal CT scans, chest X-rays, and natural background radiation in millisieverts (mSv). It demonstrates the relative radiation exposure for each imaging procedure.
The risk of developing cancer from a single CT scan is generally low, but not negligible. For most individuals, the theoretical risk of future cancer from a CT scan is estimated to be less than 0.05%, or fewer than 1 in 2,000 (1, 7). This risk is considerably lower compared to the average lifetime risk of cancer from other causes, which is about 40.14% for men and 38.7% for women (2). However, for patients who have undergone multiple CT scans, the risk can increase, ranging from 2.7% to 12% (3).
Nonetheless, it is essential to recognise that if a CT examination is clinically justified for diagnosing or evaluating treatment, the risks are negligible in comparison to the significant diagnostic benefits that CT scans offer (4, 7). Even the World Health Organization (WHO) acknowledges that the CT scan is an essential diagnostic tool that has significantly advanced patient care over time. When indicated correctly and conducted promptly, the advantages of a CT scan far surpass the associated risks (14).
MODERN CT SCANNERS AND RADIATION DOSE MANAGEMENT
Recent advancements in technology have substantially enhanced the capacity to manage radiation exposure while maintaining diagnostic accuracy.
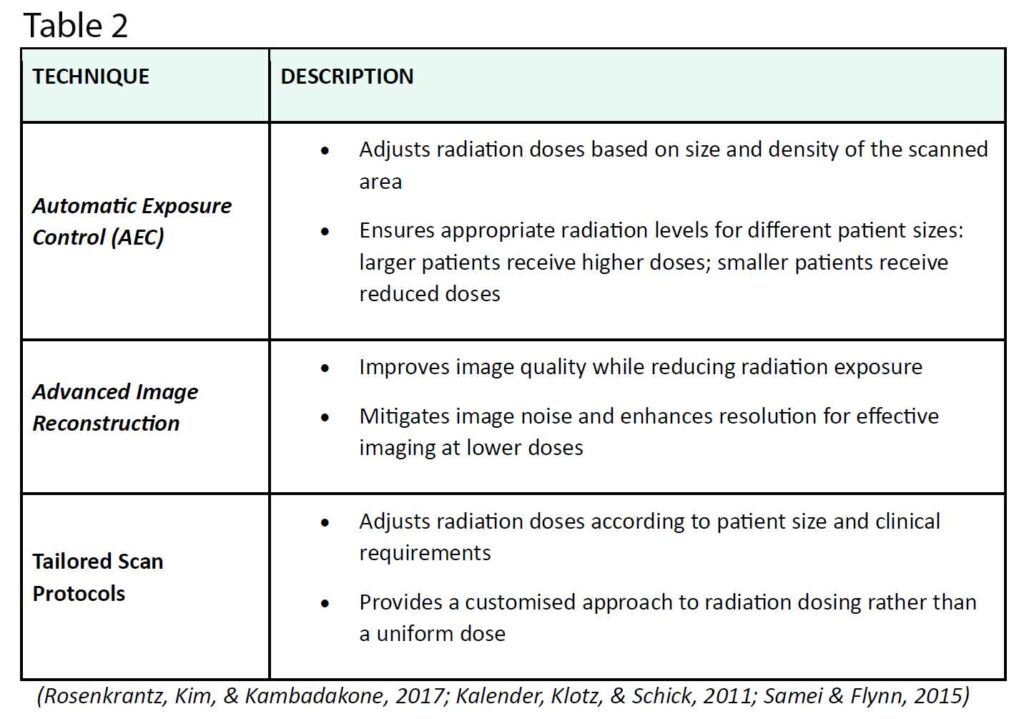
The following table provides a quick overview of how patient-specific characteristics and technology advancements are used by current CT scanners to enhance radiation dose management:
CONCLUSION
In conclusion, while the potential risks of radiation from CT scans are legitimate concerns, significant advances in CT technology have greatly improved radiation dose management. Ultimately, these developments have been shown to reduce radiation exposure while retaining high-quality diagnostic imaging. Furthermore, it is vital to assess the risks and benefits of CT scans, recognising that when used appropriately, the diagnostic benefits far outweigh the risk. Considering all of these factors, it is important for both clinicians and patients to stay informed about these developments to make well- informed decisions that optimise patient safety and care.
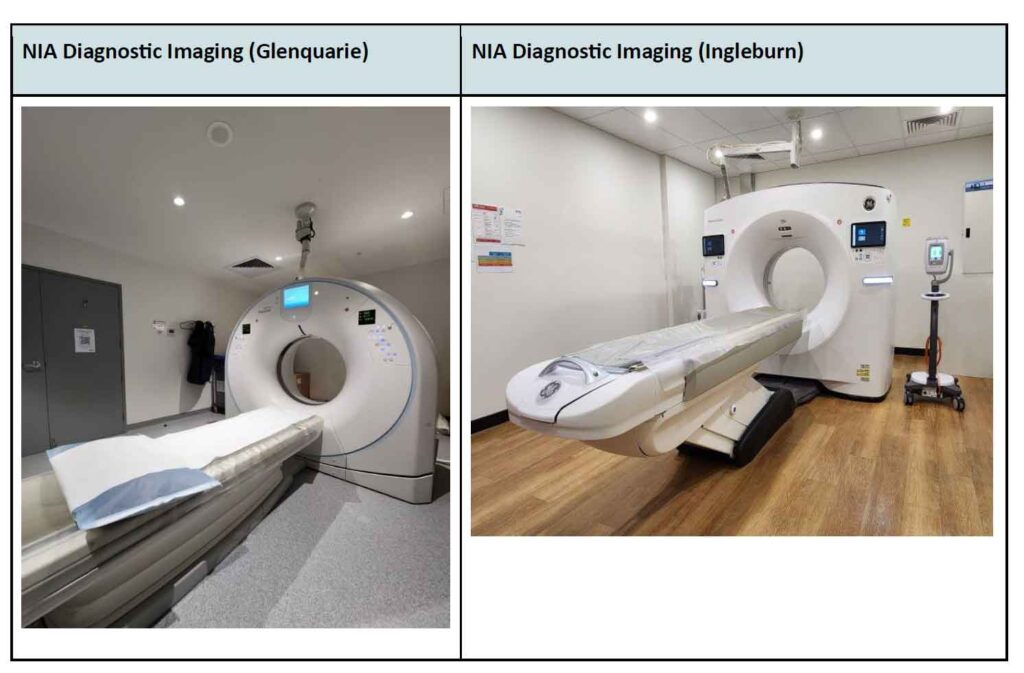
At NIA Imaging, our cutting-edge CT scanners and skilled technicians produce high-quality images while minimising radiation doses for all patients. Whether for routine or specialised imaging, NIA
Imaging is the premier choice for safe and comprehensive CT services.
REFERENCES
- Brenner, D. J., & Hricak, H. (2010). Radiation risk from medical imaging. Cancer, 116(12), 2987- 2991. https://doi.org/10.1002/cncr.25194
- Garg, M., Prabhakar, N., & Bhalla, A. S. (2021). Cancer risk of CT scan in COVID-19: Resolving the dilemma. Journal of Clinical Imaging Science, 11, 39. https://doi.org/10.25259/JCIS_29_2021
- Harvard Health Publishing. (2018, October). Radiation risk from medical imaging. Harvard Health. https://www.health.harvard.edu/cancer/radiation-risk-from-medical-imaging
- Hricak, H., Macapinlac, H., & Scardino, P. T. (2014). Imaging in oncology: Advances and challenges. The Journal of Clinical Oncology, 32(15), 1589-1600. https://doi.org/10.1200/JCO.2013.51.9811
- Johnson, T. R., Kofler, J. M., & Kambadakone, A. R. (2019). Advances in computed tomography: Innovations and clinical applications. Journal of Radiology, 26(3), 567-583. https://doi.org/10.1148/radiol.2019191921
- Kalender, W. A., Klotz, E., & Schick, M. (2011). Iterative reconstruction techniques in computed tomography: A review. Radiology, 259(2), 374-386. https://doi.org/10.1148/radiol.11102338
- Memorial Sloan Kettering Cancer Center. (2021, January 19). Scan safety: Radiation reality check. Memorial Sloan Kettering Cancer Center. https://www.mskcc.org/news/scan-safety-radiation- reality-check
- Meyer, J. W., Nitz, W. R., & Anzai, Y. (2018). Technological advances in computed tomography: Recent developments and future directions. Current Radiology Reports, 6(3), 43. https://doi.org/10.1007/s40134-018-0376-7
- Mumin, N. H., & Husain, Z. A. (2021). Computed tomography imaging in an evolving era of lung cancer screening: Opportunities and challenges. Lung India, 38(6), 548–555. https://doi.org/10.4103/lungindia.lungindia_223_21
- Rosenkrantz, A. B., Kim, D. C., & Kambadakone, A. R. (2017). Automatic exposure control in CT: Benefits and considerations. American Journal of Roentgenology, 208(2), 274-281. https://doi.org/10.2214/AJR.16.16487
- Samei, E., & Flynn, M. J. (2015). Optimization of CT scan protocols: Current trends and future directions. Journal of Medical Imaging, 2(1), 013506. https://doi.org/10.1117/1.JMI.2.1.013506
- Smith-Bindman, R., Lipson, J. A., & Marcus, R. (2009). Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Archives of Internal Medicine, 169(22), 2078-2086. https://doi.org/10.1001/archinternmed.2009.427
- Smith, J., & Doe, R. (2021). Innovations in CT imaging: From detection to guidance. Journal of Clinical Imaging Science, 11(2), 123-134. https://doi.org/10.4103/jcis.jcis_23_21
- World Health Organization. (2021). Communicating radiation risks in paediatric imaging: Information to support healthcare discussions about benefit and risk. Chapter 3: Risk-benefit dialogue. https://www.who.int/ionizing_radiation/pub_meet/chapter3.pdf?ua=1
