2nd August, 2018, Dr Chee L Khoo
I first met Jack 14 years ago when he was diagnosed with T2D from an OGTT in 2005. He was a 47 years old then. He was a busy businessman with no time for exercise and eating out fairly regularly. His BMI back then was 34.7. He was already on treatment for hypertension and dyslipidaemia. His LFTs were a little elevated with GGT 55, ALT 41. Of course, back then not much was known about non-alcoholic fatty liver and its implications.
After an initial period of close monitoring, Jack was lost to follow up for 4 years. He re-presented in 2009 with liver cirrhosis. His last diabetes check was more than a year ago. The course over the next 9 years was not unexpected – haematemesis from oesophageal varices, Transjugular Intrahepatic Portosystemic Shunt (TIPS), hepatic encephalopathy secondary to the TIPS and liver failure. The years went by and with regular tweaking, we achieved fairly decent glucose control. His HbA1c on insulin therapy sat around 6.5-7.5%.
As his liver failure progressed, his glucose control became more and more erratic. By 2014, they were working him up for a liver transplant. In the course of the investigations, a localised hepatocellular carcinoma was found but fortunately was successfully eradicated with microwave ablation.
His liver failure progress slowed and he was taken of the transplant list. His encephalopathy was now low grade. I still saw him regularly for his scripts and insulin management. His HbA1c was too low for my liking (5.8-6.2%) but he did not have signs of hypoglycaemia. He was very diligent in his SMBG with 7 readings daily. The hospital endocrinologist was “happy” with his numbers. In fact, he discharged him to my care after a couple of years. He was alive but one could hardly call that living though.
2 months ago, we organised flash glucose monitoring using the Abbott Freestyle Libre sensor. To my shock horror, he had lots of nocturnal hypoglycaemia. Over the 14-day period, we recorded 121 minutes of nocturnal hypoglycaemia some as low as 2.2 mmol/L. We quickly down titrated his insulin regimen and changed him to the newer, longer acting basal insulin.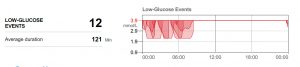
I saw Jack last week. He was a changed man. He sat up joking with me and we talked about golf, shopping and politics. He had his life back. All this time, we blamed his lack lustre existence on the encephalopathy.
A recent large scale study evaluated the link between severe hypoglycaemia and cognitive decline, brain volumes and dementia in adults with type 2 diabetes. Amongst 2001 patients with diabetes, a history of severe hypoglycaemia was associated dementia and smaller brain volume on brain MRI. Hypoglycaemia was also associated with incident dementia.
Hypoglycaemia is often hidden and patients don’t usually tell their doctors about their hypoglycaemia. A high index of suspicion is required. Further, patients with frequent hypos may not be aware of their hypoglycaemia especially, if they occur during the night. Major hypoglycaemia is also known to be associated with increased CV mortality.
There are new agents including new insulins on the market which significantly reduces the incidence of severe hypoglycaemia. A/Prof Alice Cheng from the University of Toronto, Canada is sharing her experience in the significance of hypoglycaemia and role of the new insulins. Join us here.
Reference
Lee, A.K., Rawlings, A.M., Lee, C.J. et al. Severe hypoglycaemia, mild cognitive impairment, dementia and brain volumes in older adults with type 2 diabetes: the Atherosclerosis Risk in Communities (ARIC) cohort study. Diabetologia (2018). https://doi.org/10.1007/s00125-018-4668-1
