23rd August 2019, Dr Chee L Khoo
Remember we used to have lipid targets for patients with diabetes and patients with cardiovascular disease. Life was simple then. Just follow those numbers. Then the 2013 ACC/AHA guidelines told us to throw away those targets and put everyone with cardiovascular (CV) risk above a certain figure on maximally tolerated statins. It’s kind of set and forget strategy. Not everyone accepted that dogma. The 2018 ACC have kind of backtracked a bit and we are back to some targets again. Of course, as usual, guidelines are evolving documents and they have to change when more data become available. What has changed? Let’s go back to what used to be and see what it is now.
The 2013 guidelines identified 4 major statin benefit groups for whom atherosclerotic cardiovascular disease (ASCVD) risk reduction clearly outweighs the risk of adverse effects:
- Secondary prevention in individuals with clinical events already
- Primary prevention in individuals with primary elevations of LDL-C ≥4.9 mmol/L
- Primary prevention in individuals with diabetes 40-75 years of age with LDL-C 1.8 – 4.9 mmol/L.
- Primary prevention in individuals without diabetes and with estimated 10-year ASCVD risk ≥7.5%, 40 to 75 years of age who have LDL-C 1.8 to 4.9 mmol/L.
ACC 2018 Guideline on the Management of Blood Cholesterol
Statin Benefit Group 1 – The Secondary Prevention Group
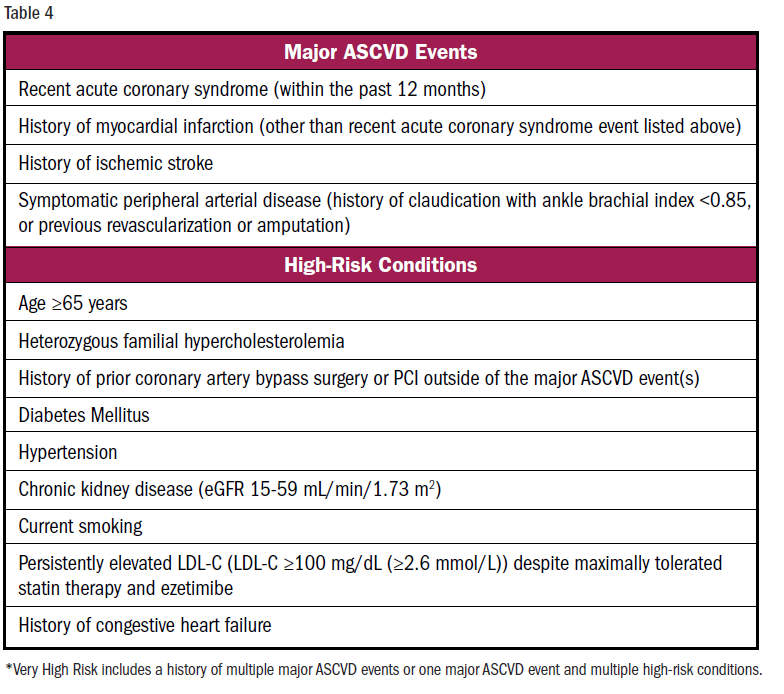
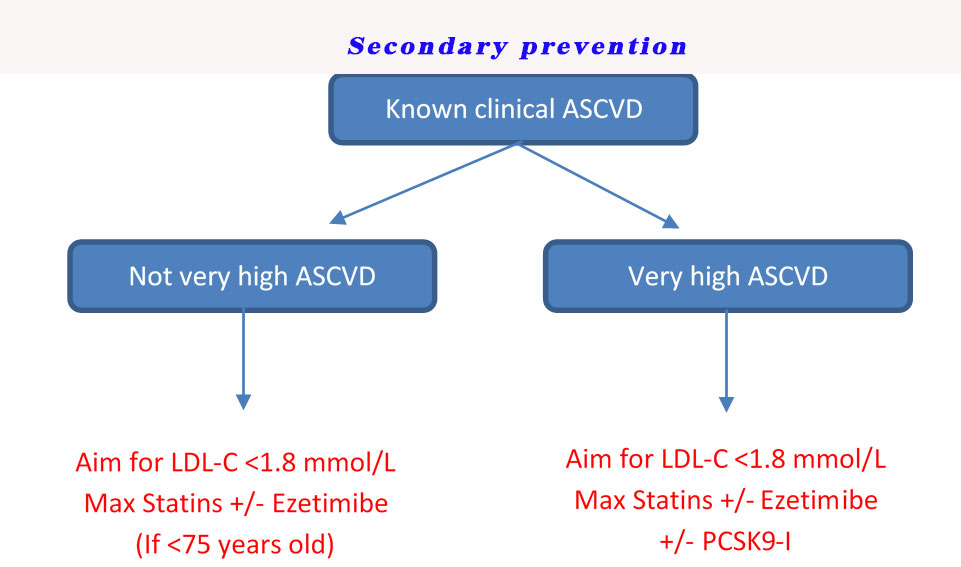
The lipid management in this group is fairly straight forward. These are patients who already have events. They are either at very high ASCVD risk or NOT at very high ASCVD risk. Patients with very high ASCVD risk are defined as patients who have multiple ASCVD or one ASCVD category plus many other risk factors. See Table 4.
Very high ASCVD risk
The recommended treatment is high intensity statins (HIS) which is either atorvastatin 80mg or rosuvastastin 40mg. The new guidelines now have an LDL-C target of 1.8 mmol/L. If maximal statins have not reduced the LDL-C to <1.8 mmol/L, there is evidence that adding ezetimibe to maximal statins have benefits. And if it still doesn’t get LDL-C <1.8 mmol/L, then consider the expensive PCSK9 inhibitors (PCSK-I).
Not very high ASCVD risk
If patients are <75 years old, then the target is still LDL-C <1.8 mmol/L. Once again adding ezetimibe to maximum statins is recommended if target is not reached (Class IIb evidence). For patients >75 years old, there is no high level evidence of adding ezetimibe to maximal statins, although recent evidence suggests that ezetimibe has benefits in patients >75 yo. As mentioned, guidelines are evolving documents and no doubt, when more evidence is available, the recommendations will change for this age group.
See Figure below.
Statin Benefit Group 2 – The Primary Prevention Group
Patients with LDL-C >4.9 mmol/L (and 20-70 years old)
Irrespective of their CV risks or associated risk enhancers, these patients need maximally tolerated statins to reduce LDL-C by >50% or <2.6 mmol/L. Add ezetimibe if targets are not achieved. Add PCSK9-I if there is familial hypercholesterolaemia and the LDL-C is still >3.4 mmol/L despite ezetimibe and maximal statins. Thus,
HIS +/- ezetimibe to get LDL-C <2.6 mmol/L
HIS +/- ezetimibe +/- bile sequestrants (if TG high) to get LDL-C <2.6 mmol/L
HIS +/- ezetimibe +/- PCSK9-I if familial hypercholesterolaemia to get LDL-C <3.4 mmol/L
Statin Benefit Group 3 – Patients with diabetes:
Patients with diabetes and LDL-C >4.9 mmol/L – these are patients in Group 2 – see above
Patients with diabetes and LDL-C 1.8-4.9 mmol/L:
40-75 years old
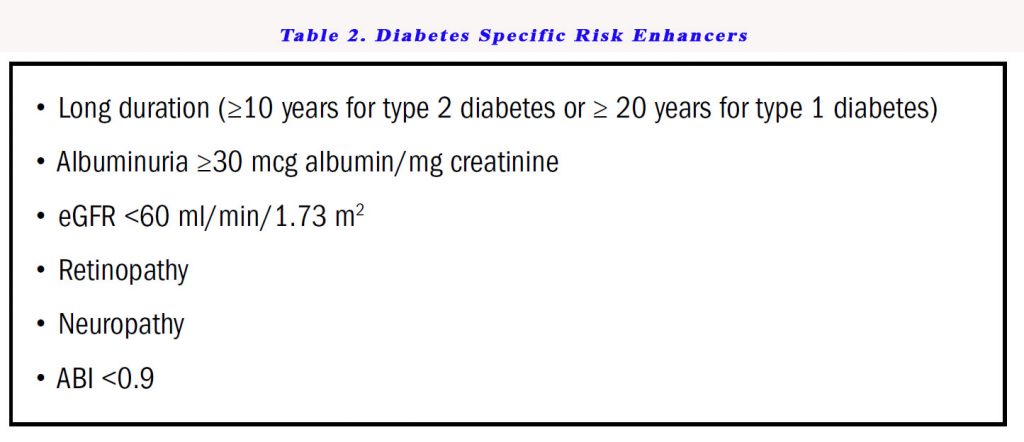
These patients require at least moderate intensity statins irrespective of CV risks. But if patients have high CV risks or have diabetes specific risk enhancers (see Table 2), they need high intensity statins to reduce LDL-C to <1.8 mmol/L especially if patients are between 50-75 years old.
In other words, pretty much all patients with diabetes need at least moderate intensity statins to reduce LDL-C by at least 30-49%. If they have diabetes risk enhancers, they need to get the LDL-C <1.8 mmol/L with maximal statins +/- ezetimibe.
<40 years old or >75 years old
There is nothing in the guidelines for these 2 groups. We are seeing more and more of these patients in our practice. I guess there are limited data out there to guide us even though it is likely that these groups have much higher and worse long-term cardiovascular outcomes. I would be inclined to treat them like those in the 40-75 year old group.
Statin Benefit Group 4 – Primary Prevention in patients with LDL-C 1.8 – 4.9 mmol/L without diabetes
0-19 years old
Lifestyle measures to reduce CVD risks
20-39 years old
Lifestyle measures to reduce CVD risks
Consider statins if there is family history or premature CVD and LDL-C >4.1 mmol/L
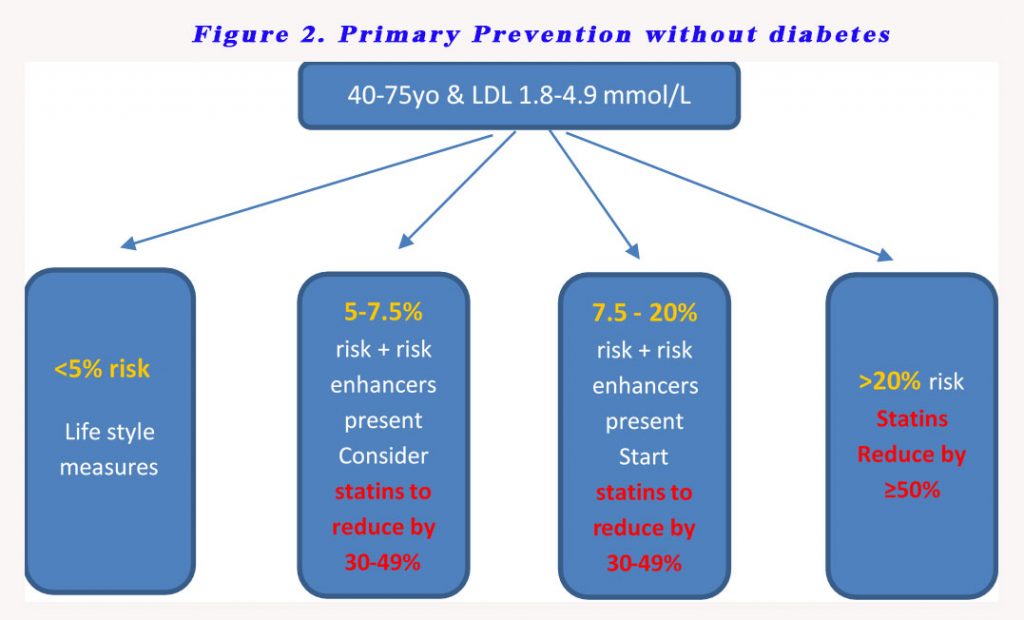
40-75 years old
Management depends on CV risks levels – see Figure 2
If after all of the above considerations and after CV risk assessment, one is still uncertain, then the guidelines recommend a coronary artery calcium score:
- CAC = zero (lowers risk; consider no statin, unless diabetes, family history of premature CHD, or cigarette smoking are present)
- CAC = 1-99 favours statin (especially after age 55)
- CAC = 100+ and/or 75th percentile, initiate statin therapy
Access the guideline here.
References:
J Am Coll Cardiol. Nov 2018; DOI: 10.1016/j.jacc.2018.11.003
