13th May 2021, Dr Chee L Khoo
The radical mastectomy introduced by Halsted was the treatment of choice for breast cancer of any size or type, regardless of the patient’s age, for 80 years. Any attempt in surgery less than a radical mastectomy was not widely considered during those years. Subsequent randomised controlled trials designed in 1969 and published in 1973 (1) and 1981 (2) showed that survival rates were equal after radical or breast-conserving surgery (BCS). BCS followed by adjuvant radiotherapy (RT) is now recommended for patients with early breast cancer. Even in patients with advanced lymph node involvement, mastectomy (Mx) does not confer any survival benefit. The criticisms of those and subsequent studies is that there are far too many confounders that may have biased the results. A recent publication examined various confounders when they compared survival after BCS and Mx.
When you think of confounding factors when comparing the two modes of treatment, you might think about the cancer type, the cancer stage, the age of the patient and perhaps, the availability of adjuvant chemotherapy or radiotherapy post operatively. There are far more complex interactions between breast cancer survival, socioeconomic status, and comorbidity.
To investigate the association of socio-economic factors and co-morbidity with overall and breast cancer–specific survival after BCS with RT, Mx with, and Mx without postoperative RT, a cohort study was conducted in Sweden (3). They collected data from all patients diagnosed as having primary invasive breast cancer from January 1, 2008, until December 31, 2017, who underwent breast surgery. The cohort was individually linked to the Swedish National Patient Registers including inpatient and outpatient care, the Cause of Death Register at the National Board of Health and Welfare, and population registers at Statistics Sweden holding demographic and socioeconomic information.
Results
Among 48 986 women, 59.9% had received BCS+RT 25.3% received Mx-RT and 14.7% received Mx+RT. At baseline, women in the BCS+RT group were more often in the Swedish mammogram screening age (40-70), had smaller tumours with less nodal involvement. Women with Mx-RT had lower education levels and a lower family income. Women in the Mx+RT had fewer HR+/ERBB2− and more high-grade tumours and were more likely to have neoadjuvant treatment, adjuvant chemotherapy and targeted treatment.
You would have thought that we need to prove that BCS+RT would be non-inferior to Mx+/-RT but the results were rather surprising. The looked at both overall survival (OS) and breast cancer specific survival (BCSS):
- In unadjusted analysis, BCS was better than either Mx+RT and Mx-RT (see Figure 1 A and 1B) in OS and BCSS
- When stratified by prognostic groups, BCS always had the highest OS and BCSS (see Figure 2)
- After adjustment for tumour stage, subtype, and grade, the associations were reduced but remained nevertheless significant
- Further adjustments for education level, family income, and country of birth and the addition of co-morbidities did not alter the estimates substantially.
- When stratifying by follow-up time, the adjusted associations for all prognostic groups combined did not vary by short (0-5 years) or long (>5 years) follow-up for overall mortality rates
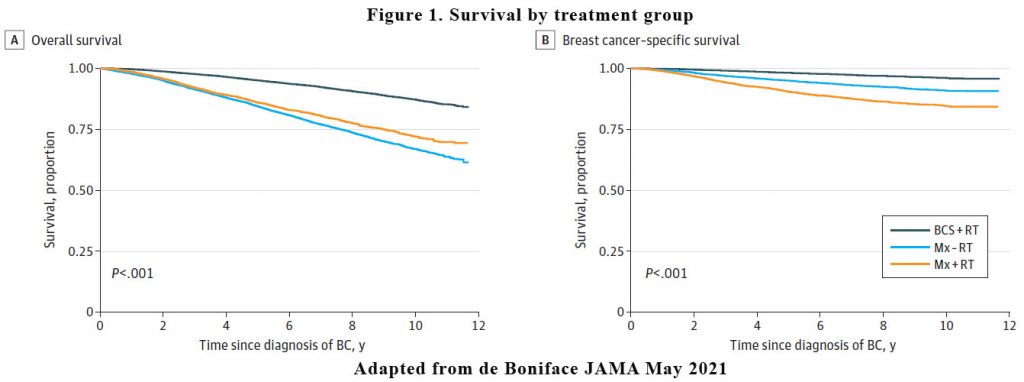
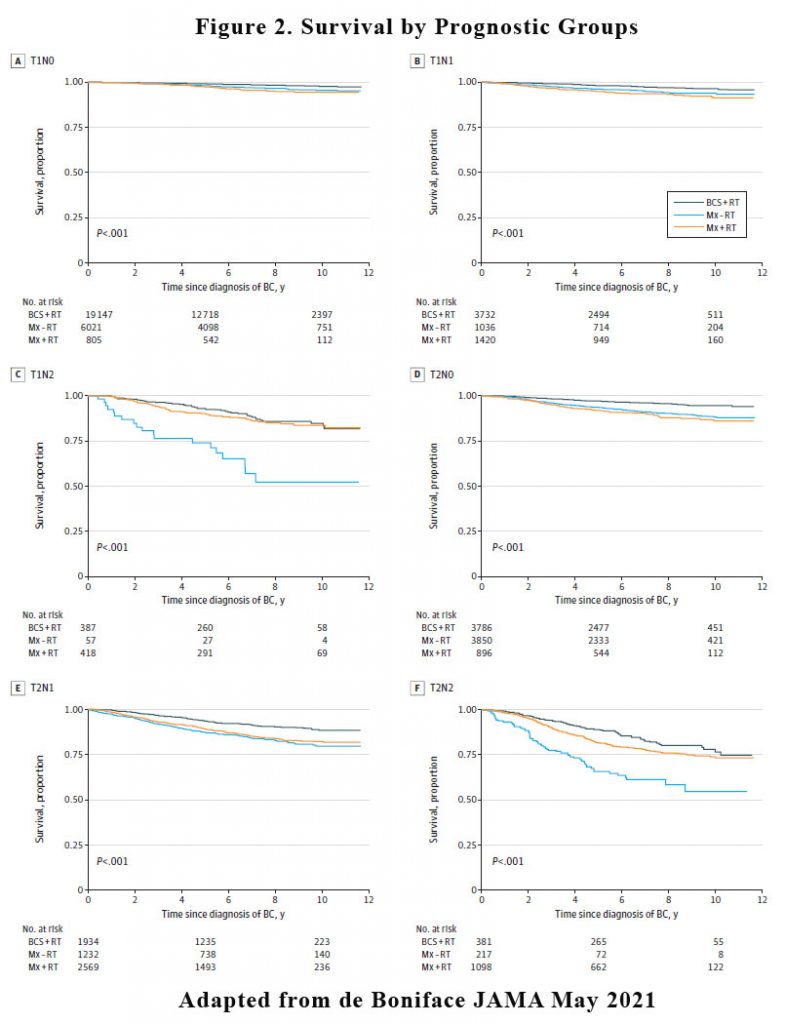
The findings of this report confirm the superiority of BCS+RT over Mx with an overall and breast cancer–specific relative survival gain of 56%to 70%in node-negative patients. The same association was observed in lower-burden, node-positive disease but not in women with higher nodal stage.
There are complex interactions between breast cancer survival, socioeconomic status, and comorbidity. Individuals with a lower socioeconomic status present with more advanced disease, have a lower adherence to mammography screening, are less likely to receive chemotherapy, and have inferior survival rates (4-6). In addition, lifestyle factors increasing cancer risk and impacting survival, such as obesity and smoking, are more common in socioeconomically deprived groups, in addition to co-morbidities that negatively affect completion rates of systemic therapy (7).
The authors did not think that BCS have some intrinsic positive association with survival, although it provides better health-related quality of life and was associated with fewer postoperative complications than Mx. This study allows us to reassure our patients that breast conserving surgery plus radiotherapy is not inferior full mastectomy with or without radiotherapy even in low burden node positive disease.
References:
- Veronesi U, Banfi A, Saccozzi R, et al. Conservative treatment of breast cancer: a trial in progress at the Cancer Institute in Milan. Cancer 1977;39:Suppl:2822-2826
- Veronesi U, Saccozzi R, Del Vecchio M, et al. Comparing radical mastectomy with quadrantectomy, axillary dissection, and radiotherapy in patients with small cancers of the breast. N Engl J Med 1981;305:6-11
- de Boniface J, Szulkin R, Johansson ALV. Survival After Breast Conservation vs Mastectomy Adjusted for Comorbidity and Socioeconomic Status: A Swedish National 6-Year Follow-up of 48 986 Women. JAMA Surg. 2021 May 5. doi: 10.1001/jamasurg.2021.1438. Epub ahead of print. PMID: 33950173.
- Lundqvist A, Andersson E, Ahlberg I, NilbertM, Gerdtham U. Socioeconomic inequalities in breast cancer incidence and mortality in Europe-a systematic review and meta-analysis. Eur J Public Health. 2016;26(5):804-813. doi:10.1093/eurpub/ckw070
- DreyerMS, Nattinger AB, McGinley EL, Pezzin LE. Socioeconomic status and breast cancer treatment. Breast Cancer Res Treat. 2018;167(1):1-8. doi:10.1007/s10549-017-4490-3
- Agarwal S, Ying J, Boucher KM, Agarwal JP. The association between socioeconomic factors and breast cancer-specific survival varies by race. PLoS One. 2017;12(12):e0187018. doi:10.1371/journal.pone.0187018
- Barnett K, Mercer SW, NorburyM,Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37-43. doi:10.1016/S0140-6736(12) 60240-2
