6th March 2022, Dr Chee L Khoo
This is about the potential cardiovascular complications after contracting covid-19 infection. It is coined “the Covid Heart”. A recent analysis of data from 154,000 US veterans one year out from their covid-19 infection have highlighted some scarry statistics. Naturally, you would expect that those who had more severe disease had higher risks of cardiovascular complications but these complications affect patients who are not hospitalised. What are the long term cardiovascular outcomes? What should we be looking out for?
The researchers examined a prespecified set of cardiovascular outcomes among patients in the US Veterans Health Administration (VHA) system who survived the first 30 days of COVID-19. They looked at the risks and excess burden of cardiovascular outcomes in 153 760 patients who used VHA services in 2019 and had a positive SARS-CoV-2 test result between March 1, 2020, and January 15, 2021 12 months after COVID-19 and compared them with two control groups:
- 5 637 647 patients with no evidence of SARS-CoV-2 infection who used VHA services in 2019—the contemporary control group
- 5 859 411 pre-pandemic patients who used VHA services in 2017—the historical control group
The cohorts largely comprised older white male patients. The COVID-19 cohort, which averaged 61 years old, included 89% males and about 71% white individuals. It also included almost 17 000 female patients; about 37 000 Black patients; and almost 8000 Latino, Asian, American Indian, Native Hawaiian, and patients of other races with COVID-19.
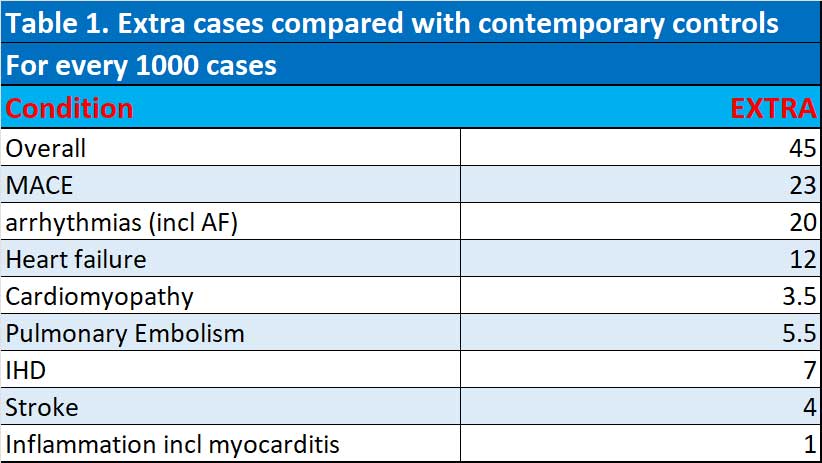
At the 12-month mark, compared with contemporary controls, for every 1000 people, covid-19 infections lead to an extra:
- 45 incidents of any prespecified cardiovascular outcome
- 23 incidents of major adverse cardiovascular events (MACEs), including myocardial infarction, stroke, and all-cause mortality
- 20 incidents of dysrhythmias, including 10.74 incidents of atrial fibrillation
- 13 incidents of other cardiovascular disorders including 12 incidents of heart failure and 3.5 incidents of nonischemic cardiomyopathy
- 10 incidents of thromboembolic disorders, including 5.5 incidents of pulmonary embolism and 4 incidents of deep vein thrombosis
- 7 incidents of ischemic heart disease including 5.5 incidents of acute coronary disease, 3 incidents of myocardial infarction, and 2.5 incidents of angina
- 5.5 incidents of cerebrovascular disorders, including 4 incidents of stroke
- 1 incident of inflammatory disease of the heart or pericardium, including 1 incident of pericarditis and 0.3 incidents of myocarditis
See Table 1.
Patients with more severe disease had higher risks. But the risks were evident even among those who were not hospitalised. The risks were increased regardless of age, race, sex, obesity, smoking, hypertension, diabetes, chronic kidney disease, hyperlipidaemia, and pre-existing cardiovascular disease.
To remove the effect of potential myocarditis from mRNA vaccination, the researchers conducted analysis to remove that effect. The increased risk of myocarditis and pericarditis remained among people who were not vaccinated and was evident regardless of vaccination status.
Implications
While the percentage of CV complications is not huge, the number of patients in practice which may have cardiovascular complications is significant when you look at the number of patients infected with covid-19 especially with the omicron wave. Covid-19 infection may lead to de novo cardiovascular disease for the first time in patients you may not think about. Cardiovascular disease is one of the organ systems affected in long Covid.
The author of the paper wrote that “early identification, diagnosis, and treatment will be key to lessening the risk of further downstream adverse health consequences.”
Reference
Abbasi J. The COVID Heart—One Year After SARS-CoV-2 Infection, Patients Have an Array of Increased Cardiovascular Risks. JAMA. Published online March 02, 2022. doi:10.1001/jama.2022.2411
