13th February 2023, NIA Diagnostic Imaging
A 30 year old woman presented to her GP with a two-day history of right sided abdominal/pelvic pain. There was associated severe nausea. On examination, there was tenderness in the right lower quadrant with guarding. A pelvic ultrasound was requested.
With this request, differential diagnosis may include haemorrhagic cyst, dermoid cyst, ovarian torsion, ectopic pregnancy or endometriosis. Another differential diagnosis is acute appendicitis.
A transabdominal and a transvaginal scan were performed revealed unremarkable uterus and ovaries. The radiologist extended the scan further to look into the right iliac fossa.
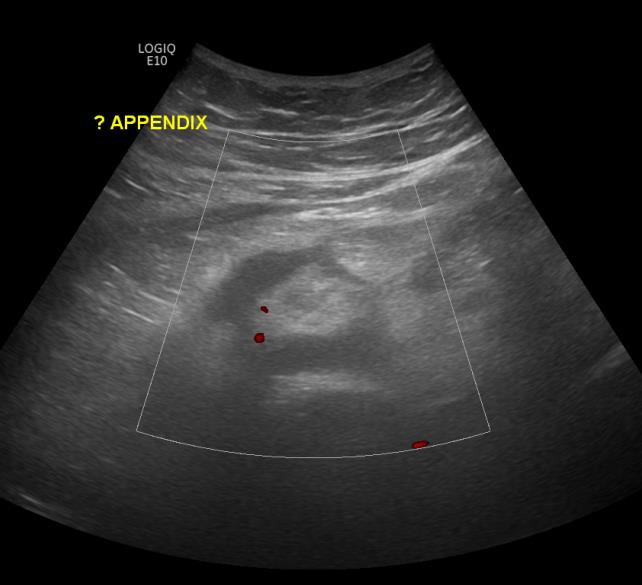
At NIA Diagnostic Imaging, we ensure we provide the best service for the patient so they receive the correct treatment. As a result, the scan was reviewed in real time by the radiologist who contacted the referring doctor to discuss and organise for a CT scan. Patient was involved in the discussion and was happy to go ahead. Results from the CT scan reported the appendix is dilated measuring 12 mm and there is stranding of the fat planes. The appearances are suggestive of acute appendicitis.

Appendicitis is an inflammation of the appendix caused by the blockage of the lumen of the appendix. (Mayo Clinic, 2019) This blockage leads to an infection as bacteria builds up within the lumen. It is considered an emergency as it can rupture causing the content to enter the abdominal cavity. This is problematic as the infected matter can cause peritonitis. (Walker 2016) Another sign is free fluid (anaechoic structure with no vascularity) in pelvis or periappendiceal area. As are enlarged lymph nodes in the abdomen or mesentery. (Bickle & Jacob 2020) A fat wrap (echogenic) may be seen around the appendix correlating to inflammatory tissue and mesentry. (Radiology Nation 2008)
For appendicitis:
- The appendix must have a diameter of >6mm proving dilation
- With defined bowel wall layers and wall thickening of >3mm
A study by Daga et.al (2017) found the sensitivity and specificity of using ultrasound to diagnose appendicitis to be 96.5% and 85.7% with a total accuracy of 95.7%. Despite this, the appendix is not always seen on ultrasound due to factors such as large habitus, bowel gas and patient compliance. A CT scan will provide a more definitive answer with its greater sensitivity. (Bickle & Jacob 2020) In this case study, there was free fluid in the RIF, a dilated tubular structure with thickened wall and surrounding echogenic mesentery. Scanning in two planes, a blind end was seen but there was some difficulty in its confirmation as it extended deep and posteriorly.
Medical technicians have a fundamental role in patient diagnosis. It is not just about the scan or performing a protocol. It is about asking the right questions and going beyond to help answer the question. Here at NIA Diagnostic Imaging, we have qualified sonographers, radiographers and radiologists performing optimal scans to deliver accurate diagnosis and excellent patient care.
References:
- Bickle, I & Jacob, K 2020, Appendicitis, Radiopaedia, viewed 21 March 2020, <https://radiopaedia.org/articles/appendicitis-2>
- Daga, S, Kachewar, S, Lakhkar, DL, Jethlia, K & Itai, A 2017, Sonographic evaluation of acute appendicitis and its complications, West African Journal of Radiology, vol. 24, no. 2, pp. 152-156
- Mayo Clinic 2019, Appendicitis, Mayo Clinic, viewed 02 April 2020, <https://www.mayoclinic.org/diseases-conditions/appendicitis/symptoms-causes/syc-20369543>
- Radiology Nation, 2018, Ultrasound Tutorial: Appendix/Appendicitis , YouTube, 14 March, viewed 31 March 2020, <https://www.youtube.com/watch?v=PfxxVXsQsfY>
- Walker, T 2016, Emergency Signs and Symptoms of Appendicitis, Healthline, viewed 30 March 2020, <https://www.healthline.com/health/digestive-health/appendicitis-emergency-symptoms>
