13th April 2023, NIA Diagnostic Imaging
A few months ago, we explored the role of coronary artery calcium score (CAC) as a cardiovascular risk assessment tool, and its importance in the prediction of future cardiovascular heart disease events and atherosclerotic cardiovascular disease (9). However, limited by the inability to assess the burden of non-calcified plaque which has low radiological attenuation, CT coronary angiography (CTCA) can be performed in conjunction with a CAC (6). So, what is CTCA? Is this CT examination useful? Does CTCA have prognostic value in patients with suspected CAD?
What is CT coronary angiography (CTCA)?
CTCA is a quick, non-invasive imaging technique that enables the visualisation of the coronary arteries with the use of iodinated contrast medium (14). With a high negative predictive value (from 92% to 99%) in the exclusion of significant CAD (11, 12), CTCA is increasingly being used to display the presence and extent of coronary atherosclerosis in symptomatic patients with suspected coronary artery disease (CAD) who are at intermediate risk of CAD after initial risk stratification (6). By identifying the site and severity of coronary lesions, CTCA can confirm or exclude CAD as the cause of symptoms such as angina, shortness or breath, or chest pain and discomfort (5) CTCA has a role in the assessment of asymptomatic patients with a strong family history of CAD.
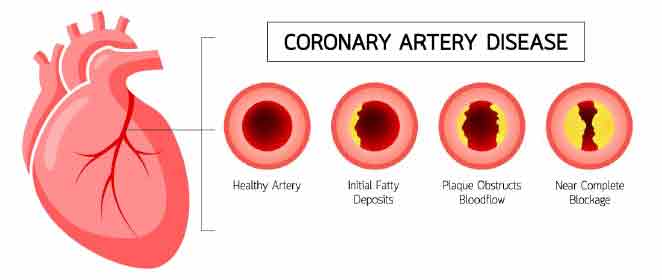
What is coronary artery disease?
In 2020, CAD was the single leading cause of disease burden and death in Australia, accounting for 10% of all deaths (3). CAD is a narrowing or blockage of the coronary arteries, often caused by a plaque buildup (5). The impaired blood flow can lead to inadequate supply of blood and oxygen to the myocardium, which over time can lead to a major adverse cardiac event such as a myocardial infarction. The risk factors for CAD include being overweight, physical inactivity, hypertension, diabetes mellitus, dyslipidaemia, smoking and family history of CAD (4). Thus, we can see that with a high prevalence of CAD, there is particular importance in diagnosis and prognosis, which can potentially impact a large proportion of individuals by guiding treatment management options and interventions.
What does the CTCA procedure involve?
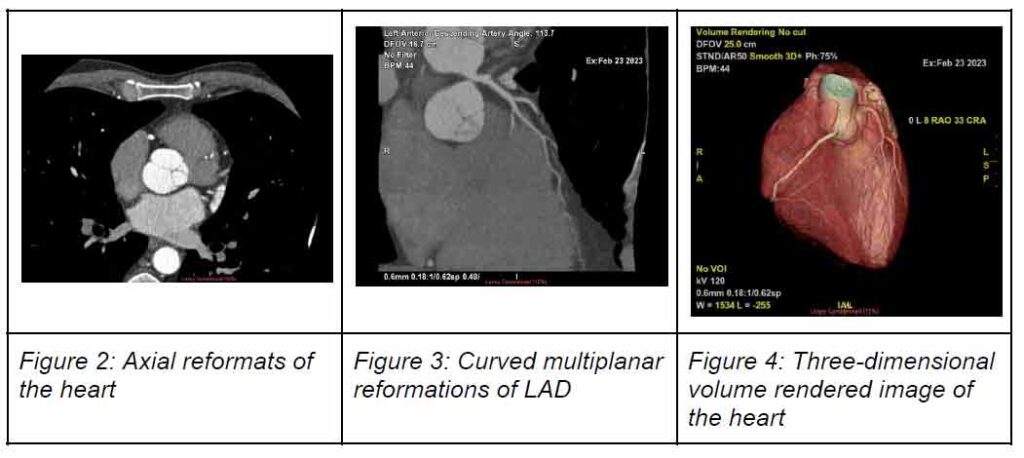
As observed in my own clinical experience, CTCA can be challenging as image quality, and thus diagnostic value, is determined by both technical and patient-related factors. Success in coronary imaging involves overcoming the effects of continuous cardiac motion to obtain images with high spatial resolution and fast temporal resolution (15). Often beta blockers such as metoprolol are prescribed to lower the heart rate, and sublingual nitrate administered to dilate the coronary arteries (15). At the conclusion of the scan, the axial CT images, curved multiplanar reformations and three-dimensional reconstructions of the heart are analysed and interpreted by a specially trained radiologist (15).
What is CTCA useful for detection of?
CTCA is useful for the accurate detection and exclusion of CAD, providing luminal stenosis assessment and characterisation of coronary atherosclerotic plaques (non-calcified, calcified and mixed) (2,12). The percentage stenosis is evaluated on curved reformats and can be classified as follows (10):
- No apparent CAD : no stenosis > 20%
- Nonobstructive CAD : ≥ 1 stenosis ≥ 20% but no stenosis ≥ 70% or left main stenosis ≥ 50%
- Obstructive CAD : any stenosis ≥ 70% or left main stenosis ≥ 50%
What is the prognostic value of CTCA?
So, does CTCA have any prognostic value? Large bodies of evidence have indicated that CTCA is increasingly used to risk-stratify in clinical practice, and has a proven prognostic value for major adverse cardiac events for patients with suspected CAD by reliably assessing atherosclerotic burden (2). Particularly among symptomatic patients, the presence of non-calcified plaque is an important predictor of future cardiac events due to its tendency to rupture, leading to acute coronary syndromes (15). In asymptomatic patients, assessment of the non-calcified plaque burden with CTCA has not been shown to improve CV risk assessment when added to CAC (6).
Normal CTCA findings with no evidence of atherosclerotic plaque confers favourable long-term prognosis during follow-up (1,2). CTCA also provides information on the presence and extent of non-obstructive CAD which may have a role in the development of acute coronary events and predictor of all-cause mortality (4). Studies have found that obstructive CAD is independently associated with an adverse outcome, and had significantly higher rates of cardiac events when compared with patients with nonobstructive CAD in relation to revascularisation and hard events (1,11).
In a study by Bittencourt et al (4), it was found that regardless of whether nonobstructive or obstructive CAD was identified, data regarding the presence, extent and severity of the disease obtained from CTCA provided additional prognostic value to the long-term prediction of cardiac death and MI, and enhanced risk assessment. By increasing the overall diagnostic rate of CAD with the use of CTCA, we can acknowledge that CTCA is a powerful tool that can impact on clinical decision-making and alter patient management pathways by targeting appropriate invasive investigations and therapeutic interventions. Two large multicentre randomised control trials (SCOT-HEART trial and PROMISE trial) demonstrated that the use of CTCA led to reductions in cardiac death from CAD and nonfatal MI than standard care alone. Furthermore, it appears that reduction in these events are attributable to the initiation of treatment interventions such as the use of aspirin and coronary revascularization procedures, cancellation of unnecessary investigations and increase in recommendations for preventive therapy such as lifestyle modifications and statin therapy (7,13).
CONCLUSION
Thus, it is highly evident that CTCA is an extremely valuable tool in the diagnosis and management of symptomatic patients with suspected CAD, and holds prognostic value for such patients. Not only does it enable risk stratification, but guide treatment management to reduce the risk of cardiac events and thus, improve quality of life for patients. CTCA examinations and calcium scoring are both offered at NIA Diagnostic Imaging, which is supervised and reported by our specially trained radiologist in cardiac image interpretation.
References:
- Aldrovandi, A., Maffei, E., Seitun, S., et al. Major adverse cardiac events and the severity of coronary atherosclerosis assessed by computed tomography coronary angiography in an outpatient population with suspected or known coronary artery disease. Journal of Thoracic Imaging, 27 (1), 23-28. doi:10.1097/RTI.0b013e3181f55d0d.
- Andreini, D., Pontone, G., Mushtaq, S., et al. A long-term prognostic value of coronary CT angiography in suspected coronary artery disease. JACC Cardiovascular Imaging, 5(7), 690–701. https://doi.org/10.1016/j.jcmg.2012.03.009
- Australian Institute of Health and Welfare. (2023). Heart, stroke and vascular disease: Australian facts . Retrieved on April 1, 2023, from https://www.aihw.gov.au/reports/heart-stroke-vascular-diseases/hsvd-facts/contents/summary-of-coronary-heart-disease-and-stroke/coronary-heart-disease
- Bittencourt, M. S., Hulten, E., Ghoshhajra, B., et al. Prognostic value of nonobstructive and obstructive coronary artery disease detected by coronary computed tomography angiography to identify cardiovascular events. Circulation Cardiovascular imaging, 7 (2), 282–291. https://doi.org/10.1161/CIRCIMAGING.113.001047
- Centers for Disease Control and Prevention. (2021). Coronary artery disease . Retrieved April 2, 2023, from https://www.cdc.gov/heartdisease/coronary_ad.htm
- Chua, A., Blankstein, R., & Ko, B. (2020). Coronary artery calcium in primary prevention. Australian Journal of General Practice, 49 (8), 464–469. https://doi.org/10.31128/AJGP-03-20-5277
- Douglas, P. S., Hoffmann, U., Lee, K. L., et al. PROMISE investigators. PROspective Multicenter Imaging Study for Evaluation of chest pain: Rationale and design of the PROMISE trial. American Heart Journal, 2014, 167 (6), 796–803.e1. https://doi.org/10.1016/j.ahj.2014.03.003
- Dugas, A. (2020). Coronary artery disease: What you need to know [Image]. Retrieved April 6, 2023, from https://ctcardio.com/cardiologist-heart-doctor/coronary-artery-disease-what-you-need-to-know/
- Khoo, C. Coronary artery calcium score – more than just a score. https://gpvoice.com.au/index.php/2022/12/18/coronary-artery-calcium-score-more-than-justa-score/
- Maddox, T. M., Stanislawski, M. A., Grunwald, G. K., et al. Nonobstructive coronary artery disease and risk of myocardial infarction. JAMA 2014, 312 (17), 1754–1763. https://doi.org/10.1001/jama.2014.14681
- Maffei, E., Seitun, S., Martini, C. Prognostic value of CT coronary angiography: Focus on obstructive vs. nonobstructive disease and on the presence of left main disease. La Radiologia Medica, 2014, 116 (1), 15–31. https://doi.org/10.1007/s11547-010-0592-2
- Mittal, T. K., Pottle, A., Nicol, E. Prevalence of obstructive coronary artery disease and prognosis in patients with stable symptoms and a zero-coronary calcium score. European Heart Journal Cardiovascular Imaging, 2017, 18 (8), 922–929. https://doi.org/10.1093/ehjci/jex037
- SCOT-HEART Investigators, Newby, D. E., Adamson, P. D., Berry, C., et al. Coronary CT angiography and 5-Year Risk of myocardial infarction. T he New England Journal of Medicine, 2018, 379 (10), 924–933. https://doi.org/10.1056/NEJMoa1805971
- Tropis, J. CT coronary angiography (CTCA). https://www.insideradiology.com.au/ctca/
- Wong, P., & Padley, S. PG. (2018). Cardiac computed tomography. Medicine, 46 (8), 474-479.
