11th June 2023, NIA Diagnostic Imaging
The incidence of pelvic organ prolapse is highly associated with increased age and vaginal childbirth (Weintraub et al., 2020). Majority of patients who present with POP may not report any symptoms. Patients who do present with symptoms, however, often describe a sense of feeling of a bulge protruding through the vaginal opening. In younger women, vaginal laxity is more commonly noticed and related to sexual dysfunction (Peter Dietz, 2015). See Table 1.

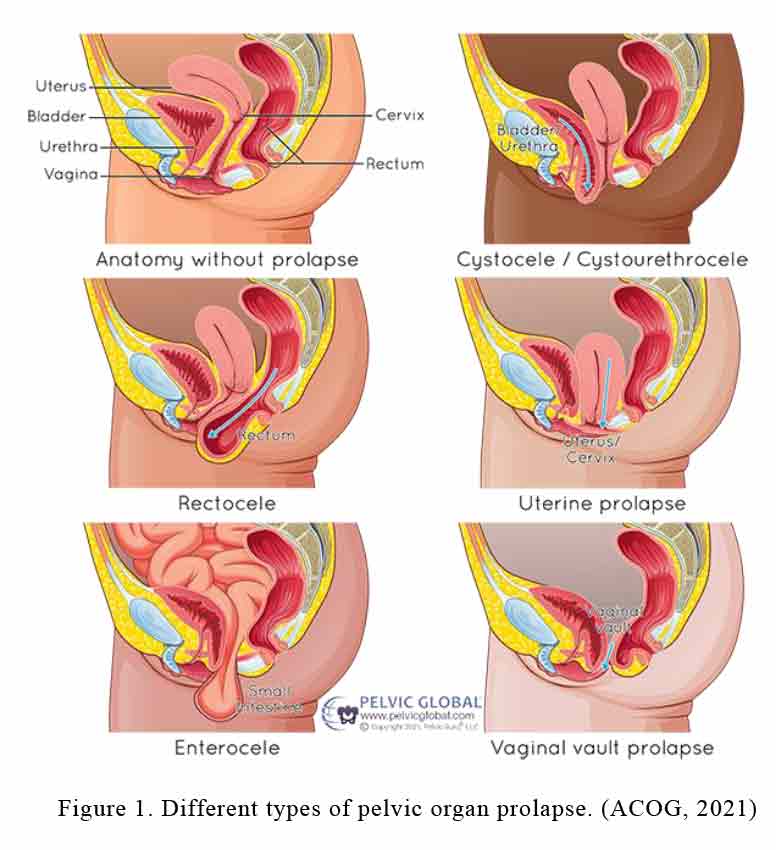
Various organs may be prolapsed (see Figure 1):
- Cystocele is the dropping of the bladder into the vagina.
- Enterocele is the bulging of the small intestine into the vagina.
- Rectocele is the bulging of the rectum into the posterior vaginal wall resulting in vaginal bulge.
- Uterine prolapse involves dropping of the uterus into the vagina.
- Vaginal vault prolapse involves the loss of vagina support and causes organs to drop out of their normal position.
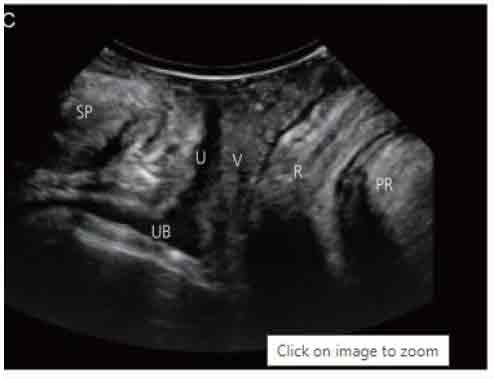
Ultrasound, when particularly performed with the translabial approach, is widely used in evaluation of women with pelvic floor dysfunction. It is a safe, simple, cost-effective and easily accessible medical imaging test. In comparison to transvaginal ultrasound imaging, the translabial approach is performed by placing the ultrasound transducer against the labia minora and urethra.
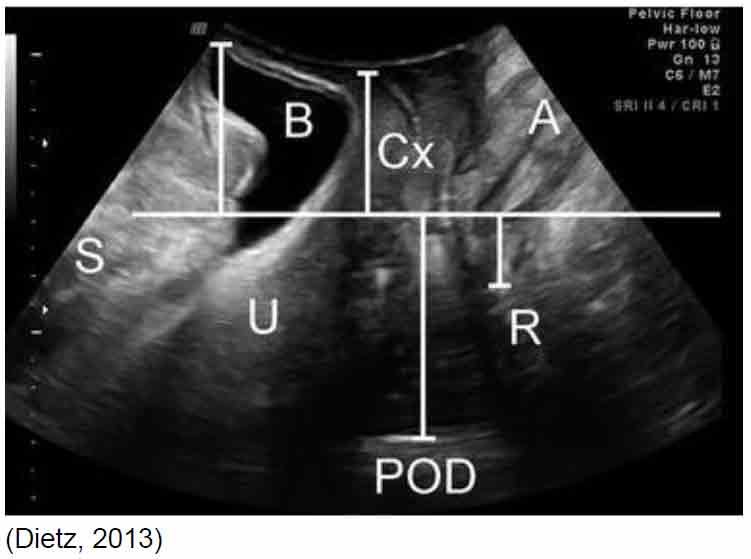
At NIA Diagnostic Imaging, the experienced sonographers, equipped with the latest GE E10 ultrasound machine, often utilise this technique to assess the pelvic organs in dynamic scan, where measurements are taken in both rest mode and under maximal Valsalva maneuver of at least 5 seconds. (Dietz, 2016). Therefore, translabial ultrasound is not only non-invasive, essentially risk-free and relatively comfortable for the patient, but also a very useful and accurate diagnostic imaging test to help confirm pelvic organ prolapse.
References
American College of Obstetricians and Gynecologists. (n.d.). Surgery for pelvic organ prolapse. ACOG. https://www.acog.org/womens-health/faqs/surgery-for-pelvic-organ-prolapse
Dietz, H. (2016). Assessment of Pelvic Organ prolapse: A Review. Ultrasound in Obstetrics & Gynecology, 48(6), 681–692. https://doi.org/https://obgyn.onlinelibrary.wiley.com/doi/full/10.1002/uog.15881
Dietz, H. P. (2013). Pelvic floor ultrasound. Current Surgery Reports, 1(3), 167–181. https://doi.org/https://link.springer.com/article/10.1007/s40137-013-0026-x
Lee, S. (2022). Translabial ultrasound for pelvic organ prolapse. Obstetrics & Gynecology Science. https://doi.org/https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10025863/
Orthopedic Physical Threapy (no date) Pelvic organ prolapse, Renew Health: Pelvic Health and Wellness. Available at: https://www.renewhealthllc.com/pelvicorganprolapse (Accessed: 08 June 2023).
Peter DIetz, H. (2015). Australian Family Physician Australian Family Physician. Pelvic Organ Prolapse – a Review, Volume 44(7). https://doi.org/https://www.racgp.org.au/afp/2015/july/pelvic-organ-prolapse-a-review
Weintraub, A. Y., Glinter, H., & Marcus-Braun, N. (2020). Narrative review of the epidemiology, diagnosis and pathophysiology of pelvic organ prolapse. International Braz j Urol, 46(1), 5–14. https://doi.org/10.1590/s1677-5538.ibju.2018.0581
