12th November 2023, NIA Diagnostic Imaging

Epigastric pain has to be one of the most common presenting symptoms in primary care. The differential diagnoses include cholelithiasis and cholecystitis. With increasing prevalence of obesity and type 2 diabetes, the prevalence of gallbladder disease is also increasing. Often, abdominal ultrasound can confirm or exclude gallbladder disease but sometimes, the results are inconclusive or we suspect additional bile duct obstruction. CT cholangiogram is a fast, widely available and non-invasive alternative technique to image the gallbladder and biliary tree [5]. This imaging technique enables three-dimensional visualisation of the detailed anatomical structures of the biliary tree including very small bile ducts such as aberrant branches [1].
Endoscopic Retrograde Cholangiography [ERC] is considered as the gold standard for visualising biliary trees [4]. However, ERC is invasive, user-dependent and can cause pancreatitis [4]. Ultrasound and MRC (MR cholangiography) are commonly used. Ultrasound is also user-dependent and the images are not easily appreciated by clinicians especially during surgical planning [4]. MRC is costly, not widely available and not suitable for patients with MRI contraindications. In MRC, the result is inconclusive if there is air within the biliary system, e.g. post Whipple’s operation and Billroth 2 [4]. Artefacts caused by surgical clips post cholecystectomy can imitate ductal cancer or a stone in MRC [4]. Therefore, CT cholangiogram utilisation should be considered.
Indications [3, 5]:
- Second line of imaging after ultrasound where the results are inconclusive
- Biliary tree obstruction
- Gallstones
- Bile duct stenosis
- Post-operative setting where bile duct injury or retained gallstones are suspected
- Patients with contraindications for MRC
Technique:
A non-contrast CT of the abdomen and pelvis is done. A second CT acquisition of the same area is done 60 minutes post drip infusion of Biliscopin (meglumine iotroxate). Biliscopin is excreted by the biliary system thus allowing for the depiction of biliary system without structural modification [1].
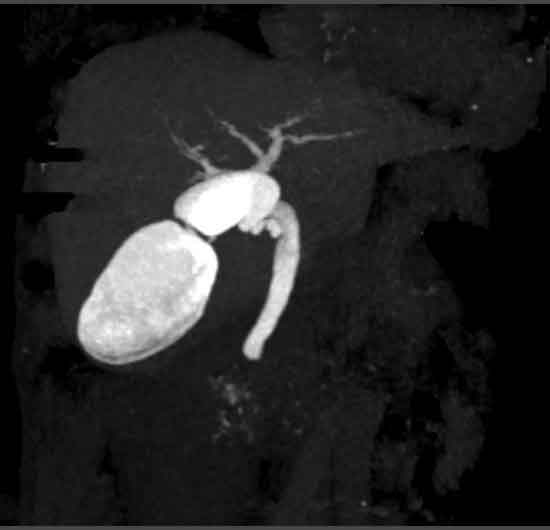
Post processing work-ups are done to produce 3D, volume rendering (VR), and maximum-intensity projection (MIP) images. 3D images allow for the depiction of the complexity of the biliary tree. VR enables specialists to stereoscopically view the path of the biliary system. MIP aids in the visualisation of small bile ducts such as aberants branches and caudate branches [1]. These anatomical variations are potential sources of surgical complications [1].
Contraindications [5]:
• Bilirubin level <30 μmol/L nor should it be rising rapidly (contrast excretion in bile is affected by the impaired excretory ability of hepatocytes)
• Severe renal or hepatic dysfunction
• Thyroid dysfunction
• Iodinated-contrast adverse reactions
Efficacy:
In the detection of choledocholithiasis, the sensitivity and specificity of CT cholangiogram are comparable to that of MRC. CT has a sensitivity of 86-93% while MRC is 80-95%. CT has a specificity of 94-100% and MRC is 88-96% [4]. Besides, CT cholangiogram is less prone to artefact than MRC [2].
In conclusion, CT cholangiogram is an excellent alternative to image the biliary system where ECR, ultrasound and MRC are not suitable or fail to give conclusive results. CT cholangiogram is cost effective, fast, widely and readily available and provides high-resolution images which assist treating clinicians in detecting a wide range of biliary system pathologies.
Case Study:
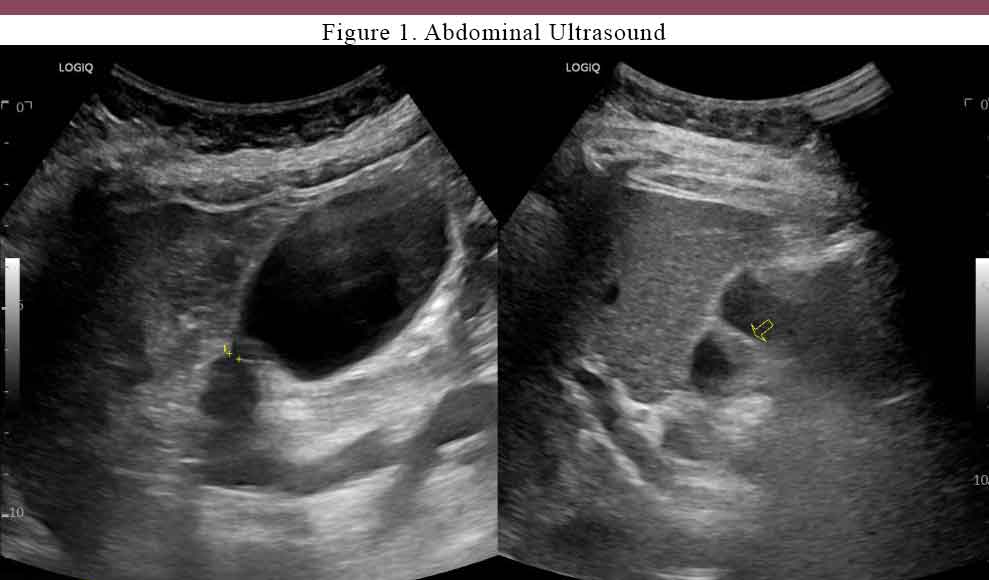
A 60-year-old patient with biliary colic and abnormal LFTs had an ultrasound of the upper abdomen at NIA Diagnostic Imaging, which showed tapering area of the gallbladder (figure 1), dilatation of the CBD and mild dilatation of the intrahepatic ducts.
A CT cholangiogram was performed at NIA later on to further investigate the cause of ductal dilatation and the tapering area. The result from the scan showed that there is mild prominence of extrahepatic ducts however, no obstruction was found as contrast can be seen in the duodenum and proximal jejunum (Figure 2-4).
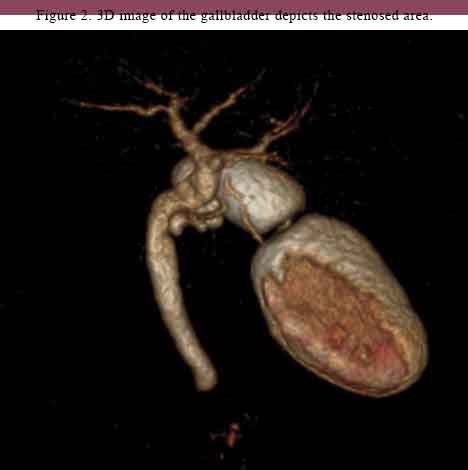
Figure 3 & 4. MIP slices show that there is no complete blockage


References:
- HYODO, T, KUMANO, S, KUSHIHATA, F, OKADA, M, HIRATA, M, TSUDA, T, … MURAKAMI, T 2012, ‘CT and MR cholangiography: advantages and pitfalls in perioperative evaluation of biliary tree’, British Journal of Radiology, vol. 85, no. 1015, pp. 887–896.
- O’Connor OJ, O’Neill S, Maher MM 2011. ‘Imaging of biliary tract disease’. AJR Am J Roentgenol, vol 197, no, 4, doi: 10.2214/AJR.10.4341
- Health South Western Sydney Local Health District, CT Cholangiogram 2015, South Western Sydney Local Health District, viewed 09 October 2023 https://www.swslhd.health.nsw.gov.au/medicalImaging/serv_CT_cholangiogram.html
- Persson, A, Dahlström, N, Smedby, O & Brismar, TB 2006, ‘Three-dimensional drip infusion CT cholangiography in patients with suspected obstructive biliary disease: a retrospective analysis of feasibility and adverse reaction to contrast material’, BMC Medical Imaging, vol. 6, no. 1, pp. 1–1.
- Weerakkody Y, Yap J, Murphy A, et al. CT cholangiography [protocol] 2023, Radiopaedia.org, viewed 09 Oct 2023 https://radiopaedia.org/articles/35600
