28th March 2024, A/Prof Chee L Khoo

We all know that when type 2 diabetes (T2D) presents at a younger age, they tend to be more aggressive in its progression as well as in the complications it causes. The complications also emerge earlier as well more aggressive. There are more cardiovascular events, more renal events and now, increasingly recognised, more liver complications. We know that patients with T2D are more likely to get hormone and non-hormone related cancers. Do the age of onset of the diabetes affect the incidence of cancers?
Studies have suggested that T2D is associated with an increased risk of liver, pancreas, endometrium, colorectum, breast, and bladder cancers and a decreased risk of prostate cancer (1). However, the evidence linking T2D and various cancers is actually very conflicting. Trying to unravel the mechanisms of the link between T2D and cancers is even more complicated with many confounding factors involved. Is it the hyperglycaemia per se or the insulin resistance that is present in many organs or the chronic inflammation that these patients have or perhaps, it is the associated metabolic derangements. It is also possible, however, that some claimed associations could be caused by biases in the literature, in particular selective reporting biases favouring the publication of significant associations and causing either false positives or inflated estimates of association (2-4).
Rentsch C et al explored one of those possible links by studying the association between HbA1c and incidence of 16 site-specific cancers within UK Biobank (5). They found a positive association between T2D and a number of cancers (colorectal, pancreatic, uterine and bladder cancer) but the association between HbA1c and cancers is only seen in pancreatic and uterine cancers. There was an inverse association with premenopausal breast cancer.
It would seem that if hyperglycaemia exposure is positively associated with cancers, then the longer the exposure is, the higher the risk would be. Young onset T2D would naturally be likely to be exposed to longer periods of hyperglycaemia. Further, as the disease is likely to be more aggressive in its progression, the degree of hyperglycaemia is also likely to be more severe.
Li Y et al recently explored the association of age at T2D diagnosis with subsequent cancer incidence in a large Chinese population (6). In a prospective population-based longitudinal cohort, 428,568 newly diagnosed T2DM patients from 2011 to 2018. All diagnosed cases of T2D is registered in the Shanghai Standardized Diabetes Management System and all cancer diagnosis is registered in the Shanghai Municipal Center for Disease Control and Prevention. Participants were divided into six groups according to their age at diagnosis: 20–54 and then at every 5 year increment to 75 years old and then >75 years old. The incidence of overall and 14 site-specific cancers was compared with the Shanghai general population including 100,649,346 person-years.
The results
The mean age of the patients with T2D were ~64 years old and not unexpectedly, the patients diagnosed less than 55 years had a higher BMI and overall, a higher fasting glucose.
T2DM patients exhibited a higher risk of pancreas, bladder, thyroid, kidney, breast, colorectum, and liver cancers compared with the general population. Amongst males with T2D, respiratory, colorectum, prostate, stomach, liver, pancreas, bladder, kidney, thyroid, and lymphoma cancers were the most frequent cancers while amongst females, breast, respiratory, colorectum, thyroid, pancreas, stomach, liver, CNS, gallbladder, and uterine cancers were the most frequent cancers.
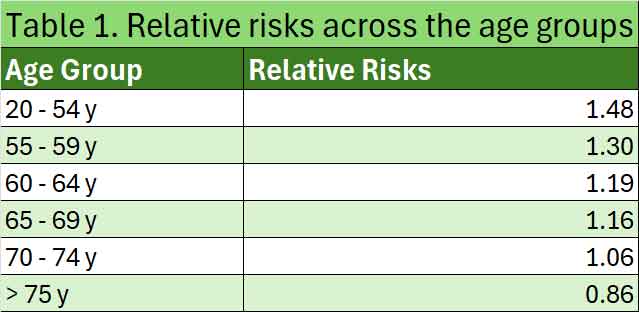
Younger age at T2DM diagnosis was associated with higher incidence of overall and site-specific cancers. SIRs for overall cancer with T2DM diagnosis at ages 20–54, 55–59, 60–64, 65–69, 70–74, and > 75 years were 1.48 (1.41, 1.54), 1.30 (1.25, 1.35), 1.19 (1.15, 1.23), 1.16 (1.12, 1.20), 1.06 (1.02, 1.10), and 0.86 (0.84, 0.89), respectively. See Table 1.
Similar trends were observed for site-specific cancers, including respiratory, colorectum, stomach, liver, pancreatic, bladder, central nervous system, kidney, and gallbladder cancer and lymphoma among both males and females.
The higher incidence of cancers in patients with T2D have previously been reported. However, few studies explicitly considered the association between cancer incidence and age at diabetes diagnosis. One prospective study with 125 all-cause cancer cases illustrated a mildly elevated risk of cancer in women with diabetes onset earlier in childhood (7). Studies of specific types of cancer suggested that early-onset diabetes confers a higher relative incidence of pancreatic cancer and colon cancer than late-onset diabetes (8,9).
The potential reasons for the excess risk of cancer is unclear. Accumulating data suggest that young-onset T2D has a more rapid deterioration of b-cell function than that in later-onset T2DM (10-13). It is likely that exposure to high glucose is a risk factor, earlier studies show that young people with T2DM had higher fat content in liver and muscle, in association with higher BMI and Homeostatic Model Assessment for Insulin Resistance, than that in older adults with T2D (11).
We also know that high BMI is associated with higher risk of certain cancers, notably thyroid cancer in all patients, breast and uterine cancer in female patients, and prostate cancer in male patients.
This study reminds us of a number of issues. When we are managing patients with young onset T2D, managing the metabolic derangements including obesity and insulin resistance is just as important as managing glycaemia. As young onset T2D is likely to have a longer duration of the disease in the future, we need to be more aggressive in our management. The findings of this study remind us that we also need to be more on the lookout for various cancers.
References:
- Giovannucci E, Harlan DM, Archer MC, Bergenstal RM, Gapstur SM, Habel LA, et al. Diabetes and cancer: a consensus report. Diabetes Care2010;33:1674-85.
- Dwan K, Altman DG, Arnaiz JA, Bloom J, Chan AW, Cronin E, et al. Systematic review of the empirical evidence of study publication bias and outcome reporting bias. PLoS One2008;3:e3081
- Ioannidis JP. Why most published research findings are false. PLoS Med 2005;2:e124.
- Ioannidis JP. Why most discovered true associations are inflated. Epidemiology 2008;19:640-8.
- Rentsch CT, Farmer RE, Eastwood SV, Mathur R, Garfield V, Farmaki AE, Bhaskaran K, Chaturvedi N, Smeeth L. Risk of 16 cancers across the full glycemic spectrum: a population-based cohort study using the UK Biobank. BMJ Open Diabetes Res Care. 2020 Aug;8(1):e001600. doi: 10.1136/bmjdrc-2020-001600
- Li Y, Tian J, Hou T, Gu K, Yan Q, Sun S, Zhang J, Sun J, Liu L, Sheng CS, Pang Y, Cheng M, Wu C, Harris K, Shi Y, Bloomgarden ZT, Chalmers J, Fu C, Ning G. Association Between Age at Diabetes Diagnosis and Subsequent Incidence of Cancer: A Longitudinal Population-Based Cohort. Diabetes Care. 2024 Mar 1;47(3):353-361. doi: 10.2337/dc23-0386. PMID: 38237119
- Fredriksson M, Persson E, Dahlquist G, M€ollsten A, Lind T. Risk of cancer in young and middle-aged adults with childhood-onset type 1 diabetes in Sweden–a prospective cohort study. Diabet Med 2022;39:e14771
- Gupta S, Vittinghoff E, Bertenthal D, et al. New-onset diabetes and pancreatic cancer. Clin Gastroenterol Hepatol 2006;4:1366–1372; quiz 1301
- Ali Khan U, Fallah M, Sundquist K, Sundquist J, Brenner H, Kharazmi E. Risk of colorectal cancer in patients with diabetes mellitus: A Swedish nationwide cohort study. PLoS Med 2020;17:ce1003431
- Viner R,White B, Christie D. Type 2 diabetes in adolescents: a severe phenotype posing major clinical challenges and public health burden. Lancet 2017;389:2252–2260
- Lascar N, Brown J, Pattison H, Barnett AH, Bailey CJ, Bellary S. Type 2 diabetes in adolescents and young adults. Lancet Diabetes Endocrinol 2018;6:69–80
- Wang T, Lu J, Shi L, et al.; China Cardiometabolic Disease and Cancer Cohort Study Group. Association of insulin resistance and b-cell dysfunction with incident diabetes among adults in China: a nationwide, population-based, prospective cohort study. Lancet Diabetes Endocrinol 2020;8:115–124
- Fan B,Wu H, Shi M, et al. Associations of the HOMA2-%B and HOMA2-IR with progression to diabetes and glycaemic deterioration in young and middle-aged Chinese. Diabetes Metab Res Rev 2022;38:e3525
