13th July 2024, NIA Diagnostic Imaging
Preterm birth/labour (PTL) is the most common cause of neonatal mortality and morbidity. Preterm birth is defined as delivery prior to 37 weeks of gestation (1). In Australia, the preterm birth rate ranges from 8.3% in 2011 and 8.2% in 2021 with the highest in recent years at 8.7% in 2018 (2). Transvaginal ultrasound (TVUS) is considered as the gold standard in the measurement of cervical length (CL) and is routinely used as part of preterm labour’s risk assessment (4).
Indications for TVUS cervical length measurement in pregnancy (7):
- CL <35mm on transabdominal ultrasound (TAUS)
- Cervix is not well visualised on TAUS
However, TVUS is invasive and is often described as uncomfortable by patients (8,9). Contraindications of TVUS according to the ASA includes (10):
- No consent obtained from patient
- Cannot be done if high risk of labour is suspected
Other considerations where TVUS can be done but with great caution:
- Placenta praevia +/- per vaginum (PV) bleeding. TVUS should be used discriminately and care must be taken during the advancement of the transducer into the vagina. The relationship between the tip of the transducer and the cervix should be continually assessed in real time.
- PPROM (premature rupture of membrane) was considered a contraindication for TVUS as it may pose a risk of infections and reduce the latency period. A small study has shown that TVUS does not increase these risks. However, with little evidence and study available, the decision to use TVUS is dependent on the obstetric care provider and local protocols.
Thus, an alternative technique should be considered in the case when TVUS is contraindicated. Transperineal ultrasound (TPUS) is a non-invasive technique with high correlation to TVUS and is preferred by pregnant women in multiple research studies (5).
TPUS technique:
- Informed consent must be obtained.
- A low-frequency linear array transducer (4-7 MHZ) with sterile probe cover and gel are used.
- The patient is scanned with an empty bladder in a lithotomy position with the hips elevated on a cushion to reduce rectal gas over the external os (7).
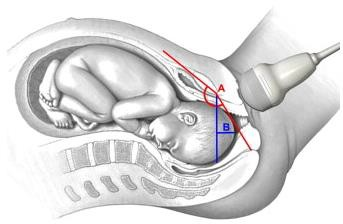
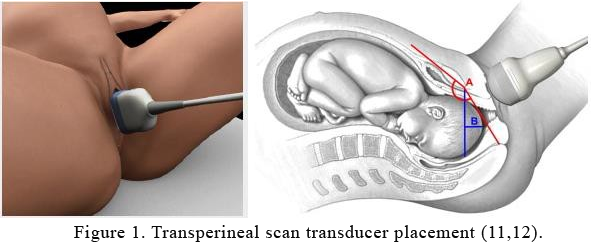
- The transducer is placed externally on the labia or perineum, just posterior to the symphysis pubis in a mid-sagittal plane along the direction of the vagina (Figure 1).
- The transducer is moved in oblique or parasagittal until the cervical canal, external and internal ora are in view (5, 6).
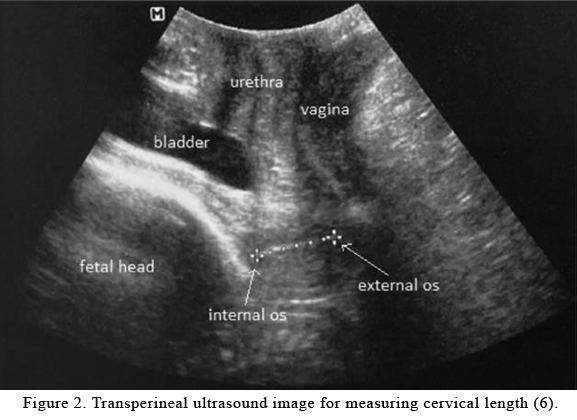
- Cervical length measurement is done by placing the callipers at the internal and external ora (5) as shown in figure 2.
Advantages of TPUS
- No additional ultrasound transducer required (3)
- TPUS is non-invasive as it avoids direct contact with the cervix (3)
- More comfortable and tolerable than TVUS (5)
- Its non-invasive nature reduces
the risk of (3)
- Infection
- Bleeding in the case of placenta previa
- Inaccurate measurement due to probe pressure in TVUS. This can lead to overtreatment and iatrogenic results or under treatment and preterm birth
- Triggering emergency episodes such as rupture membranes or cord prolapse
Reliability of TPUS
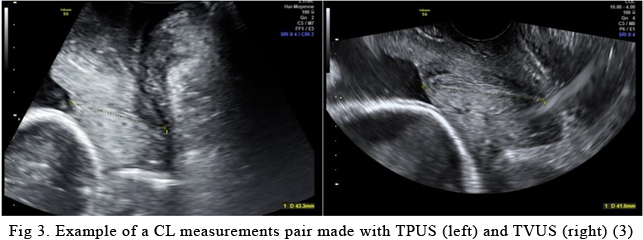
- TPUS has a 95% sensitivity and a 100% specificity (3)
- High correlation with TVUS with interobserver reliability (5)
- Estimated difference in CL measurements between TVUS and TPUS was only 0.2mm (5)
Limitation of TPUS
- Shadowing caused by pubis symphysis or/and bowel gas. However, elevating the hips can reduce this issue (5).
- The inexperience of sonographers. However, this can be eliminated with training (6).
In conclusion, transperineal ultrasound has proven to be a suitable alternative technique in cervical length measurement in obstetric ultrasound.
At NIA Diagnostic Imaging, our sonographers are highly proficient and dedicated to obtaining optimal sonographic images for precise diagnosis. We recognise that transvaginal ultrasound may not be suitable for every female patient’s comfort. Therefore, we are committed to employing alternative techniques to ensure comprehensive measurements and scans, prioritising patient comfort throughout the process.
References
- RANZCOG, 2021, “Measurement of cervical length for prediction of preterm birth”, RANZCOG, viewed 5th July 2024, <https://ranzcog.edu.au/wp-content/uploads/2022/05/Measurement-of-cervical- length-for-prediction-of-preterm-birth-C-Obs-27_Board-approved-March-2022.pdf >
- AIHW, 2023, Australia’s mothers and babies, AIHW, viewed 5th July 2024 <https://www.aihw.gov.au/reports/mothers-babies/australias-mothers-babies/contents/summary>
- Krief, D, Foulon, A, Tondreau, A, Diouf, M, Sergent, F, Gondry, J & Chevreau, J 2023, ‘Transperineal ultrasound in routine uterine cervix measurement’, Archives of Gynecology and Obstetrics, vol. 307, no. 2, pp. 387–393.
- Clinical Trial: Evaluation of Transperineal Ultrasound Technic for Diagnostic Shorted Cervical Length for Pregnant Women (2nd and 3rd Trimester) Compared to Endovaginal Technic (Gold Standard) 2020, US Fed News Service, Including US State News, HT Digital Streams Limited, Washington, D.C.
- Songserm, V, Komwilaisak, R, Saksiriwuttho, P & Kongwattanakul, K 2019, ‘Transperineal versus transvaginal sonographic measurements of cervical length in pregnant women between 16 and 24 weeks of gestation’, Journal of Clinical Ultrasound, vol. 47, no. 7, pp. 389–393.
- Ho, KKW, Wong, CK, Hung, CMW & Lau, WL 2024, ‘Transperineal ultrasound measurement of cervical length to predict preterm delivery in women with threatened preterm labour’, Hong Kong Journal of Gynaecology, Obstetrics, and Midwifery = Xianggang Fu Chan Zhu Chan Ke Za Zhi, vol. 24, no. 1, pp. 8–12.
- Newnham JP, White SW, Meharry S, Lee HS, Pedretti MK, Arrese CA, Keelan JA, Kemp MW, Dickinson JE, Doherty DA. Reducing preterm birth by a statewide multifaceted program: an implementation study. Am J Obstet Gynecol 2017;216(5):434-42
- Meijer-Hoogeveen M, Stoutenbeek P, Visser GH. Methods of sonographic cervical length measurement in pregnancy: a review of the literature. J Matern Fetal Neonatal Med 2006;19:755-62
- Larscheid P, Maass N, Kennes LN, Najjari L (2015) Transperineal ultrasound to measure cervical length of pregnant women in general and in particular with cervical insufciency—a comparison of transabdominal and transperineal ultrasound as alternatives to transvaginal ultrasound. Ultraschall Med 36:59–64
- Thoirs, K, O’Hara, S, Quinton, A, Coombs, P, Srayko, S, Spurway, J, … O’Brien, S 2024, ‘Ultrasound assessment of the gravid cervix to assess for risk of spontaneous preterm birth: Introducing an evidence‐based clinical guideline for sonographers’, Sonography, vol. 11, no. 2, pp. 113–125.
- Salsi G, Cataneo I, Dodaro G, Rizzo N, Pilu G, Sanz Gascòn M, Youssef A. Three-dimensional/four- dimensional transperineal ultrasound: clinical utility and future prospects. Int J Womens Health. 2017;9:643-656. https://doi.org/10.2147/IJWH.S103789
- Amin, M. A., Eltomey, M. A., & El-Dorf, A. A. (2014). Role of transperineal ultrasound measurements in women with prolonged second stage of labor as predictors of the mode of delivery. Egyptian Journal of Radiology and Nuclear Medicine, 45(4), 1295–1299. https://doi.org/10.1016/j.ejrnm.2014.05.01
