28th February 2025, A/Prof Chee L Khoo

Every so often you come across a study where the initial and immediate impression is that there must be more to the conclusion. The latest study which connects the use of anti-depressants with further cognitive decline in patients with dementia is just one of those studies. Now, many patients who have dementia also have depression and are on anti-depressants and we don’t think twice about whether the drugs might hasten the decline in cognitive function in these patients. But then, patients who are depressed and receiving SSRIs/SNRIs are also more likely to develop dementia (1). So, how do you unravel the connections between the dementia, depression and anti-depressants?
In the latest study published in the BMC Medicine Journal, Minjia Mo et al looked at patients with dementia registered in the Swedish Registry for Cognitive/Dementia Disorders-SveDem from May 1, 2007, until October 16, 2018, with at least one follow-up after dementia diagnosis, and who were new users of antidepressants (2). They excluded patients with antidepressant dispensation prior to the 6-month period before the date of dementia diagnosis and patients who received prescriptions for different antidepressants within a class or antidepressants from different classes in the same 6-month period. This was obviously, designed to remove the confounding effect of depression per se contributing to cognitive decline.
The primary outcome for this study was cognitive decline, defined as mini-mental state examination (MMSE) score change over the years. The secondary outcomes included severe dementia, fracture, and death.
Results
18,740 patients were included in this cohort study of which 4271 (22.8%) received at least one prescription for an antidepressant. The total number of person-years of follow-up was 80,737, with a mean (SD) of 4.3 (2.2) years per patient.
During follow-up, a total of 11912 prescriptions for antidepressants were issued, with selective serotonin reuptake inhibitors (SSRI) being the most common (64.8%), followed by tricyclic antidepressants (TCAs) (2.2%), serotonin noradrenaline reuptake inhibitors (SNRIs) (2.0%), and the group of other antidepressants (31.0%). Antidepressant use was associated with faster cognitive decline compared with non-use. See Figure 1.
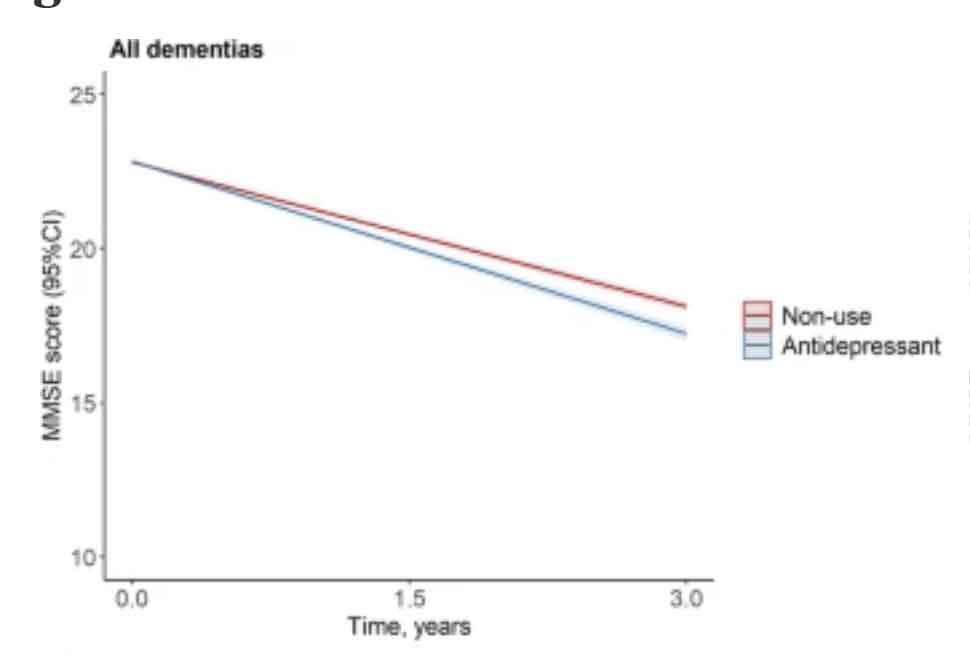
Amongst the different SSRI/SNRI, in order of speed of decline, the worse was escitalopram (MMSE score change: − 0.76 points/year), followed by citalopram (− 0.41points/year), sertraline (− 0.25 points/year), and mirtazapine (− 0.19 points/year) compared with non-use. Higher dispensed doses of antidepressants, specifically for SSRIs and the group of other antidepressants were associated with faster cognitive decline during follow-up.
The results were largely similar for AD and mixed dementia (β = − 0.28 points/year), vascular dementia (β = − 0.27 points/year), and other dementias (β = − 0.34 points/year) but not lewi-body dementia (LBD) and frontotemporal dementia (FTD). A slower cognitive decline was observed in younger (< 78 years) patients with FTD (β = 1.61 points/year. The association was stronger in patients with severe dementia (initial MMSE scores 0–9).
The results were similar whether patients were on cholinesterase inhibitors or not.
Compared with non-use, antidepressant use was also associated with higher risk of all-cause mortality (HR = 1.07) and fracture (HR = 1.18). Higher dispensed dose of SSRIs were associated with increased risk of severe dementia (HR = 1.35), all-cause mortality (HR = 1.18), and fracture (HR = 1.25) compared with non-use.
This is one of many studies on the relationship between antidepressant use and cognitive decline. Previous studies of antidepressant use and cognitive decline in people with dementia have shown mixed findings. the majority of the cases reported, antidepressants had the same effect on cognition as placebo [3-6], but some reported a significant decline on the MMSE scores in antidepressant users [7,8]. A recently conducted RCT reported worsening of cognition in patients with AD who used citalopram over 9 weeks [3]. In contrast, other RCTs in AD indicated that another two SSRIs, sertraline and escitalopram, had no effect on cognitive function [9,10].
Relevance to our practice
This study sought to see the independent effect of anti-depressants in causing further cognitive decline. They tried to isolate the effect of anti-depressants on dementia by excluding patients who already have depression at the time of diagnosis. The cognitive declined associated with antidepressants as shown in this study were very small. This study also found slower cognitive decline in younger (< 78 years) patients with FTD.
Not all patients with dementia have depression. Antidepressants don’t seem to work as well in patients with dementia because depression in dementia is a different illness than depression in people with intact cognition [11]. Sometimes, anti-depressants might be used to manage agitation, behaviour issues and sleep disturbance.
The findings of this study might help us choose the SSRI with lesser impact on cognitive decline. There were slight increases in mortality and fracture risks in those on anti-depressants compared with non-use. We need to think twice before we initiate anti-depressants or least consider reducing their falls risk as well a review of their cardiovascular risks.
References:
- Wang GHM, Chen WH, Chang SH, Zhang TX, Shao H, Guo JC, Lo-Ciganic WH. Association between first-line antidepressant use and risk of dementia in older adults: a retrospective cohort study. Bmc Geriatrics. 2023;23(1).
- Mo, M., Abzhandadze, T., Hoang, M.T. et al. Antidepressant use and cognitive decline in patients with dementia: a national cohort study. BMC Med 23, 82 (2025).
- Dudas R, Malouf R, McCleery J, Dening T. Antidepressants for treating depression in dementia. Cochrane Database Syst Rev. 2018;8(8):CD003944.
- Maier F, Spottke A, Bach JP, Bartels C, Buerger K, Dodel R, et al. Bupropion for the Treatment of Apathy in Alzheimer Disease: A Randomized Clinical Trial. JAMA Netw Open. 2020;3(5): e206027.
- Mowla A, Mosavinasab M, Haghshenas H, Borhani HA. Does serotonin augmentation have any effect on cognition and activities of daily living in Alzheimer’s dementia? A double-blind, placebo-controlled clinical trial. J Clin Psychopharmacol. 2007;27(5):484–7.
- Qin M, Wu J, Zhou Q, Liang Z, Su Y. Global cognitive effects of second-generation antidepressants in patients with Alzheimer’s disease: A systematic review and meta-analysis of randomized controlled trials. J Psychiatr Res. 2022;155:371–9.
- Porsteinsson AP, Drye LT, Pollock BG, Devanand DP, Frangakis C, Ismail Z, et al. Effect of citalopram on agitation in Alzheimer disease: the CitAD randomized clinical trial. JAMA. 2014;311(7):682–91.
- Teri L, Logsdon RG, Peskind E, Raskind M, Weiner MF, Tractenberg RE, et al. Treatment of agitation in AD: a randomized, placebo-controlled clinical trial. Neurology. 2000;55(9):1271–8.
- Choe YM, Kim KW, Jhoo JH, Ryu SH, Seo EH, Sohn BK, et al. Multicenter, randomized, placebo-controlled, double-blind clinical trial of escitalopram on the progression-delaying effects in Alzheimer’s disease. Int J Geriatr Psychiatry. 2016;31(7):731–9
- Munro CA, Longmire CF, Drye LT, Martin BK, Frangakis CE, Meinert CL, et al. Cognitive outcomes after sertaline treatment in patients with depression of Alzheimer disease. Am J Geriatr Psychiatry. 2012;20(12):1036–44.
- Alexopoulos GS, Manning K, Kanellopoulos D, McGovern A, Seirup JK, Banerjee S, Gunning F. Cognitive control, reward-related decision making and outcomes of late-life depression treated with an antidepressant. Psychol Med. 2015;45(14):3111–20
