12th December 2019, Dr Chee L Khoo
Type 2 diabetes (T2D) and heart failure (HF) are common diseases with significant morbidity and mortality. Two out of three patients with T2D have evidence of ventricular dysfunction within 5 years of diabetes diagnosis (1). Data from both observational studies and clinical trial cohorts suggest that the development of HF in patients with T2DM is associated with anywhere from a 4- to 10-fold increase in mortality risk (2,3). The risk of HF in patients with T2DM persists even when traditional cardiovascular risk factors, such as smoking, hypertension, and low-density lipoprotein cholesterol, are well controlled (4). SGLT2 inhibitors have been shown in a number of clinical trials to reduce the risk of hospitalisation for heart failure. If only we can identify patients with T2D who are at high risk of heart failure. Can we?
The Saxagliptin Assessment of Vascular Outcomes Recorded in Patients With Diabetes Mellitus–Thrombolysis in Myocardial Infarction 53 (SAVOR-TIMI 53) and Dapagliflozin Effect on Cardiovascular Events – Thrombolysis in Myocardial Infarction 58 (DECLARE – TIMI 58) trials were multinational, randomised, placebo-controlled trials enrolling patients with T2DM and either a history of established cardiovascular disease or multiple risk factors for cardiovascular disease. In the SAVOR-TIMI 53 trial, 79% of subjects had established cardiovascular (CV) diseases and 21% had multiple risk factors while in the DECLARE-TIMI 58, 41% of subjects had established CV diseases and 59% had multiple risk factors.
A multivariable clinical risk score for HHF in patients with T2D enrolled in the placebo arm of SAVOR-TIMI 53 trial have been created (6). The score have been validated in placebo treated patients in the DECLARE -TIMI 58 trial. 25 risk factors were initially selected based on their prevalence, clinical relevance, and the ability to readily obtain the variables from the medical records of typical patients with T2D. These included age, sex, race, body mass index, duration of T2DM, HbA1c, baseline insulin use, history of diabetic retinopathy, history of diabetic nephropathy, estimated glomerular filtration rate (eGFR), urine albumin-to-creatinine ratio (UACR), established CAD, previous MI, established peripheral artery disease, previous ischemic stroke, pre-existing HF, history of atrial fibrillation, previous percutaneous coronary intervention, previous coronary artery bypass grafting, dyslipidemia, hypertension, current smoking, heart rate, systolic blood pressure, and diastolic blood pressure.
Each of the 25 risk factors were evaluated to determine their association with the development of hospitalisation for heart failure in the SAVOR-TIMI 53 trial. All risk indicators achieving a significance level of P<0.10 on the univariable screen were included in a multivariable model. Out of the 25 risk factors, 5 independent factors were found to achieve statistical significance in their association with HHF. They were included in the final risk score, The TIMI Risk Score for Heart Failure (TRS-HFDM). These variables were:
- History of HF,
- History of atrial fibrillation,
- Coronary artery disease (CAD),
- eGFR <60 mL/min/1.73 m2, and
- UACR >35 mg/mmol
They used the TRS-HFDM to internally validate their model. They then used the score on placebo patients from the DECLARE-TIMI 58 trial. eGFR and UACR were found to have such strong association with HHF that their presence carried extra weighting in the score (see below).
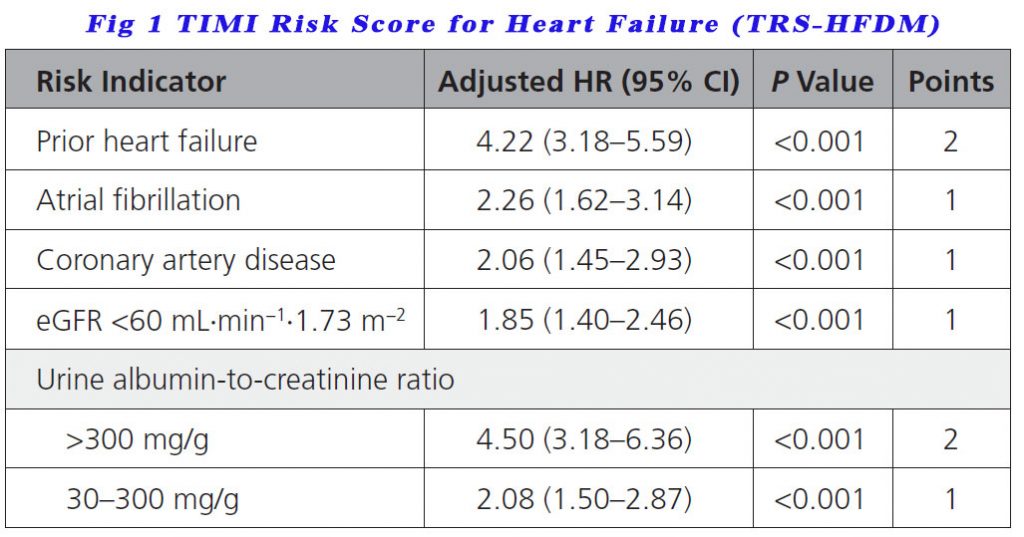
300 mg/g converts to 35 mg/mmol (approximately)
Patients scoring 0 points were low risk of developing HF, those with 1 point were in intermediate risk, those with 2 points were high risk while those with 3 points or more were classed as very high risk.
Heart failure does not often come with symptoms. A risk scoring system is useful to trigger screening for heart failure in patients with T2D and concomitant cardiac and/or renal disease. Far more important though is that with the TRS-HFDM scoring, we can see who may benefit most from an SGLT2 inhibitor like dapagliflozin which is what the scoring study was based on.
The relative risk reductions were similar across the risk categories but the absolute risk reduction (ARR) was higher with higher risk categories. Patients with low, intermediate, high, and very high risk of HHF had ARRs of 0.3%, 0.6%, 1.5%, and 2.7% respectively, which translates into numbers needed to treat of 303, 172, 65, and 36 respectively, to prevent 1 HF hospitalisation at 4 years.
One could also use the scoring system to avoid saxagliptin in patients with high to very high risk of HHF.
TIMI Risk Score for Heart Failure (TRS-HFDM) is an excellent yet simple clinical risk prediction tool which has excellent discrimination, is well calibrated, and can help clinicians counsel patients about their risk of HHF and identify those patients at higher risk for HHF who have a greater absolute reduction in HHF risk with SGLT2 inhibitors.
References
- Shah et al. Lancet Diabetes Endocrinol. 2015; 3(2):105–113.
- Bertoni AG, Hundley WG, Massing MW, Bonds DE, Burke GL, Goff DC Jr. Heart failure prevalence, incidence, and mortality in the elderly with diabetes. Diabetes Care. 2004;27:699–703. doi: 10.2337/diacare.27.3.699
- Carr AA, Kowey PR, Devereux RB, Brenner BM, Dahlöf B, Ibsen H, Lindholm LH, Lyle PA, Snapinn SM, Zhang Z, et al. Hospitalizations for new heart failure among subjects with diabetes mellitus in the RENAAL and LIFE studies. Am J Cardiol. 2005;96:1530–1536. doi: 10.1016/j.amjcard.2005.07.061
- Rawshani A, Rawshani A, Franzén S, Sattar N, Eliasson B, Svensson AM, Zethelius B, Miftaraj M, McGuire DK, Rosengren A, et al. Risk factors, mortality, and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2018;379:633–644. doi: 10.1056/NEJMoa1800256
- Kamalesh & Cleophas. J Card Fail. 2009; 15(4):305–9.
- David D. Berg, Stephen D. Wiviott, Benjamin M. Scirica et al. Heart Failure Risk Stratification and Efficacy of Sodium-Glucose Cotransporter-2 Inhibitors in Patients With Type 2 Diabetes Mellitus. Circulation. 2019;140:1569–1577. DOI: 10.1161/CIRCULATIONAHA.119.042685
