!2th March 2021, Dr Chee L Khoo
A substantial number of myocardial infarctions (MIs) are asymptomatic (silent MI (SMI)) or associated with minor and atypical symptoms and are found accidentally during routine electrocardiogram (ECG) examinations that reveal the existence of abnormal Q waves. The risk factors for occurrence of SMI are increasing age, hypertension, existing coronary artery disease and diabetes. Remember a few months ago when Medicare cut rebates and restricted our access to cardiac investigations including ECG and stress testing? The bureaucrats seem to think that “routine” ECG is a waste of time. How else are you going to detect SMI? In most studies, there is no difference in the risk of a major cardiovascular events compared with clinical MI. What about other ECG abnormalities short of infarct on the ECG? Do they help identify those at risk of major cardiovascular events?
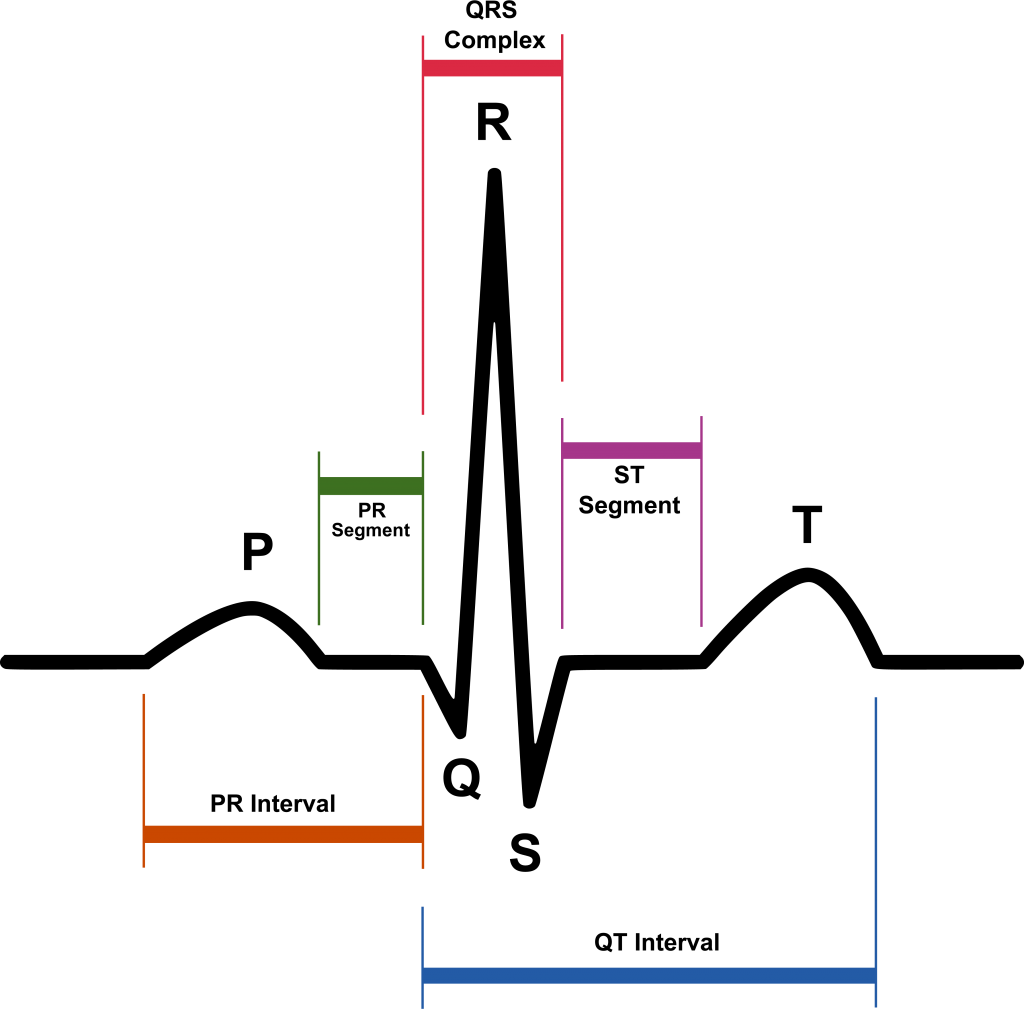
The T-wave is the repolarization of the ventricles. T wave changes including low-amplitude T waves and abnormally inverted T waves may be the result of many cardiac and non-cardiac conditions. The normal T wave is usually in the same direction as the QRS except in the right precordial leads. Also, the normal T wave is asymmetric with the first half moving more slowly than the second half. In the normal ECG, the T wave is always upright in leads I, II, V3-6 and always inverted in lead aVR.
T-wave abnormalities (TWA) are a common ECG abnormality encountered during routine clinical practice with an estimated prevalence of 1.3% of the general population [1, 2]. In the absence of known clinical cardiovascular disease, these TWA are often non-specific and of uncertain significance. While major ECG abnormalities such as ST segment elevations and Q-waves have been shown to be associated with subsequent clinical cardiovascular events, the prognostic importance of TWA has not been fully established [3]. This importance of TWA is particularly uncertain in individuals with no history of clinical CVD who are found to have incidental TWA on routine ECG.
TWA was found in studies to be associated with increased risk of all-cause mortality and cardiac mortality but subjects usually have ST elevation myocardial infarction, arrhythmia or heart failure.
Among patients with diabetes, there is limited data about the prognostic significance of TWA.
In a recent study, data from the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial and the ACCORDION follow-up study was utilised to explore the relationship between TWA and subsequent clinical cardiovascular events in patients with diabetes (4,6). Now, the ACCORD trial is a multicentre randomised clinical trial of patients with diabetes and CVD designed to assess the effect of various strategies of glycaemic, BP and lipid control on cardiovascular mortality. In the ACCORDION follow-up study, the original participants continued to be followed for up to 14 years from the start of ACCORD.
Subjects who had baseline ECG of adequate T-wave analysis were included in this analysis. The magnitude of the TWA was correlated to the risk of averse cardiovascular events which included all-cause mortality, cardiovascular mortality, congestive heart failure (CHF), major CHD (a composite of death from CHD, nonfatal myocardial infarction and unstable angina) and stroke.
The study found that compared with the reference group of participants with no TWA, participants with minor TWA had increased risk of all-cause mortality, cardiovascular mortality, CHF and major CHD. Similarly, participants with major TWA had even higher risk of all-cause mortality, cardiovascular mortality, CHF and major CHD when compared with no TWA as well as minor TWA.
Interestingly, TWA in the anterolateral leads (I, aVL, V6) as well as inferior leads (II, III, aVF) were associated with higher risk of all-cause mortality, cardiovascular mortality, CHF and major coronary
artery heart disease, while TWA in the anterior leads (V2-V5) alone did not have statistically significant associations with cardiovascular events.
There are a limited number of studies that have explored TWA in the general population without a history of CHD, and these studies are of smaller sample sizes. One such study included men who did not have known heart disease and followed them for a mean of 21 years, finding that TWA was associated with increased CHD-related death as well as all-cause mortality [5].
The presence and magnitude of TWA are associated with increased risk of clinical cardiovascular
events and mortality in individuals with diabetes and may have value in refining risk, particularly in those with prevalent CVD.
If only we can convince the bureaucrats of the value of routine ECG screening in patients with higher risk of CV events.
References:
- Aro A, Anttonen O, Tikkanen J et al (2012) Prevalence and prognostic significance of T-wave inversions in right precordial leads of a 12-lead electrocardiogram in the middle-aged subjects. Circulation 125(21):2571–2577
- Krittayaphong R, Muenkaew M, Chiewvit P, Ratanasit N, Kaolawanich Y, Phrommintikul A (2019) Electrocardiographic predictors of cardiovascular events in patients at high cardiovascular risk: a multicenter study. J Geriatr Cardiol 16(8):
- Holkeri A, Eranti A, Haukilahti MAE, Kerola T, Kenttä TV, Tikkanen JT, Anttonen O, Noponen K, Seppänen T, Rissanen H, Heliövaara M, Knekt P, Junttila MJ, Huikuri HV, Aro AL. Predicting sudden cardiac death in a general population using an electrocardiographic risk score. Heart. 2020 Mar;106(6):427-433. doi: 10.1136/heartjnl-2019-315437. Epub 2019 Nov 15. PMID: 31732657.
- Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, Byington RP, Goff DC Jr, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH Jr, Probstfield JL, Simons-Morton DG, Friedewald WT. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008 Jun 12;358(24):2545-59. doi: 10.1056/NEJMoa0802743. Epub 2008 Jun 6. PMID: 18539917; PMCID: PMC4551392.
- Kurl S, Mäkikallio TH, Laukkanen JA (2015) T-wave inversion and mortality risk. Ann Med 47(1):69–73. https://doi.org/10.3109/07853890.2014.985703
- Mould SJ, Soliman EZ, Bertoni AG, Bhave PD, Yeboah J, Singleton MJ. Association of T-wave abnormalities with major cardiovascular events in diabetes: the ACCORD trial. Diabetologia. 2021 Mar;64(3):504-511. doi: 10.1007/s00125-020-05337-8. Epub 2021 Jan 8. PMID: 33420509.
