28th March 2024, A/Prof Chee L Khoo
We all know that high LDL-C is absolutely and adversely associated with cardiovascular mortality and morbidity. It’s been “proven” again and again in large clinical trials and meta-analyses after meta-analyses. Reducing lipids levels have also been shown to reduce cardiovascular (CV) events in secondary as well as in primary prevention. This is particularly the case in those with intermediate to high CV risks. Patients with diabetes are at nearly double the risk for atherosclerotic cardiovascular disease (ASCVD) compared with those without diabetes (1). According to national and international guidelines, patients with intermediate or higher CV risks need to be on at least moderate-intensity statins.
We touched on the importance of treating dyslipidaemia almost 2 years ago here. There are actually 4 steps to managing lipids in patients with diabetes: 1) Assess CV risk (cvdcheck.org.au or MESA CV risk score calculator) 2) Decide on dosage of statins necessary for the task 3) determine the target LDL-C to aim for 4) Determine what other agents is necessary to get to target LDL-C.
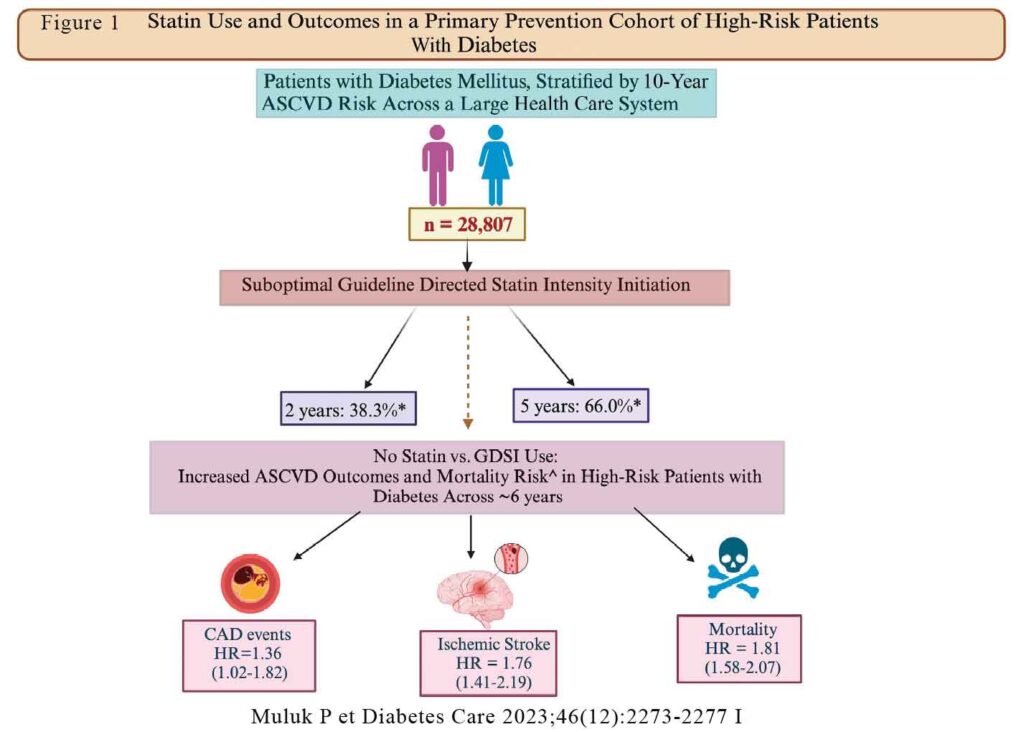
What if they are not treated according to guideline-directed statin-intensity (GDSI)? Muluk P et al recently examined cardiovascular outcomes in patients with T2D who were on GDSI compared with those who were not on GDSI (2). They looked at adults 20-79 years old within the University of Pittsburgh Medical Center (UPMC) health care system. These are patients who did not have established ASCVD. So, it’s about primary prevention of CVD.
The results
Out of 282,298 eligible primary prevention patients, 27032 patients had T2D. The mean age were 57 years old. At baseline, only 49.5% intermediate-risk and 53.4% high-risk patients were receiving GDSI therapy. Over an ~6-year follow-up period, only ~ 70% of patients with diabetes were prescribed any statin therapy, of whom only ~50% achieved GDSI (moderate- or high-intensity statin therapy). The mean time to achieve GDSI was ~2 years after the first encounter within the system.
Compared with patients without diabetes, patients with diabetes had a higher risk of incident CAD (HR 1.76 [95% Cl 1.49-2.08]; P < 0.05] and stroke (1.44 [1.20-1.731), even with GDSI use. However, for all-cause mortality, GDSI use decreased this risk compared with no statin (1.31 vs. 2.38, respectively; P < 0.001).
In particular, over the 6-year follow-up period, compared with patients with diabetes receiving GDSI therapy, patients with diabetes not on any statins had a lower risk for 36% higher risk of incident CAD, 76% higher risk of stroke, and 81% higher risk of all-cause mortality. See Figure 1.
There may be a number of reasons why patients with diabetes are not on GDSI when they should be. Approximately 5-30% of patients taking a statin experienced statinassociated muscle symptoms (14), leading to statin intolerance. Whether this is true intolerance or not is hard to tell but this is a real cause of non-adherence. There may be due to a lower perceived CV risk by the physician leading to clinical inertia.
In summary, there is still a large gap in GDSI use in high risk patients with diabetes. This places patients are significantly higher adverse ASCVD outcomes which can be avoided. Are you complicit to your patients experiencing a CVD event?
References:
- Saeed A, Ballantyne CM. Assessing cardiovascular risk and testing in type 2 diabetes. Curr Cardiol Rep 2017;19:19
- Muluk P, Zhu J, Thoma F, Hay E, Marroquin O, Makani A, Aiyer A, Nasir K, Gulati M, Shapiro MD, Mulukutla S, Saeed A. Impact of Guideline-Directed Statin Intervention for Primary Prevention in Patients With Diabetes. Diabetes Care. 2023 Dec 1;46(12):2273-2277. doi: 10.2337/dc23-0816. PMID: 37851356.
