27th October 2024, A/Prof Chee L Khoo
Patients with heart failure have high mortality and morbidity. Each time they are admitted into hospital with an exacerbation, their cardiac function deteriorate and usually do not return to pre hospital level when they are better. Many of these patients have other co-morbidities which can mask their symptoms or they are in and out of hospital with the other co-morbidities that the HF is overlooked. When the patient is symptomatic and in acute cardiac decompensation, the diagnosis is usually straight forward but in patients with minimal or no symptoms, diagnosis can be challenging. This is where biomarkers such as serum natriuretic peptides, NTpro-BNP or BNP can be useful. Up until now, those tests are not funded by Medicare. It is funded now.
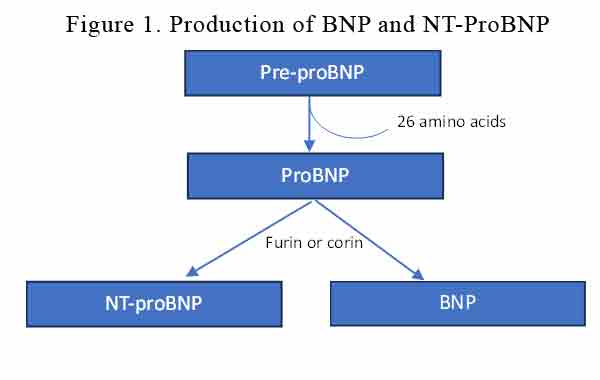
We comprehensively review the utility of NP 15 months ago. With Medicare funding available now, it is worthwhile revisiting this important biomarker. Brain Natriuretic peptide (BNP) is produced primarily by ventricular cardiomyocytes in response to volume or pressure overload. BNP and NT-proBNP are synthesised from a pre-hormone (pre-proBNP). Pre-proBNP is cleaved off into proBNP which is converted into NT-proBNP and BNP by furin or corin. See Figure 1.
BNP and NT-proBNP levels are normally very low but their levels increase when the cardiomyocytes are under stress as in heart failure or in atrial fibrillation. It is an attempt by the body to improve the haemodynamics by arterial vasodilation, diuresis, and natriuresis. It is also meant to exert anti-hypertrophic and anti-fibrotic effects, and counteracts the activation of RAAS, SNS and the endothelin systems.
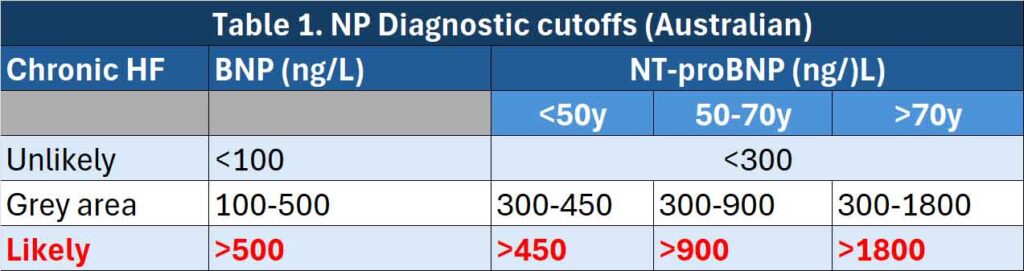
Like any other diagnostic tests, we need to consider the sensitivity and specificity of BNP and NT-proBNP in the diagnosis of heart failure. The criteria for diagnosis is different for acute heart failure and chronic heart failure, different age groups and whether the patient is in the community (mostly asymptomatic) or presenting in emergency departments (mostly symptomatic).
European Society of Cardiology (ESC) guidelines recommend the use of BNP and NT-proBNP for the exclusion of HF with reference values < 100 ng/L and < 300 ng/L for acute HF, respectively, and < 35 ng/L and < 125 ng/L for chronic HF, respectively (1).
Our Australian laboratory reference ranges for BNP and NT-proBNP are (2,3):
BNP has a shorter half-life than NT-proBNP. Circulating BNP levels are like NT-proBNP in normal individuals but are significantly less elevated by left ventricular dysfunction. BNP levels may be elevated by factors other than CHF, such as acute coronary syndrome, pulmonary embolism, shock, atrial arrhythmia, severe pneumonia and renal disease. BNP levels are higher in women than men, increase with age and have an inverse relationship with BMI (lower in obesity).
NT-proBNP has a longer half-life than BNP. Circulating levels are like BNP in normal individuals, but are significantly more elevated by left ventricular dysfunction than BNP. NT-proBNP levels may be elevated by factors other than CHF, such as acute coronary syndrome, pulmonary embolism, shock, atrial arrhythmia, severe pneumonia and renal disease. NT-proBNP levels are higher in women than men, increase with age and have an inverse relationship with BMI (lower in obesity).
See Table 1.
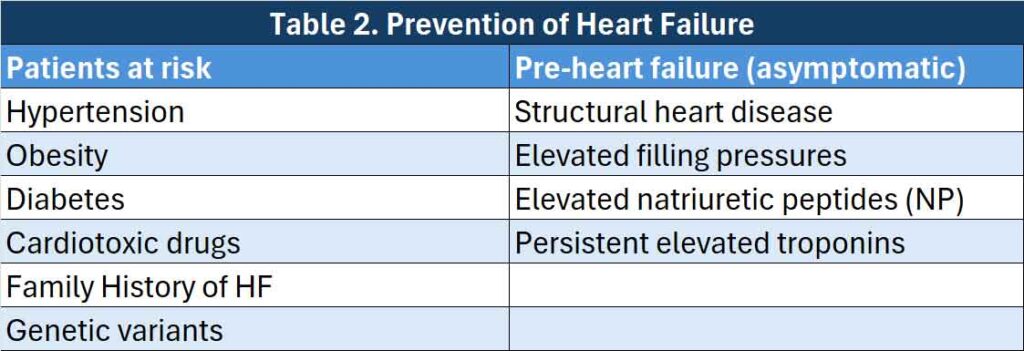
Why should we screen with NP?
While we now have the four pillars of treatment for patients with heart failure with reduced ejection fraction (HFrEF) and have a number of pharmaceutical agents shown to reduce hospitalisation for heart failure and CV mortality in both HFrEF and heart failure with preserved ejection fraction (HFpEF), there is a need to get in early both with early diagnosis and prevention of heart failure before it becomes symptomatic. We need to target those at risk of heart failure and those who has evidence of heart failure but asymptomatic (so-called pre-heart failure). This is where our serum biomarkers become most useful. The ACC/AHA guidelines suggest that NPs should be used to screen subjects at risk of developing HF to optimise medical therapy and prevent LV dysfunction (4). See Table 2.
From the 1st November 2024, serum BNP and NT-proBNP is Medicare rebatable naturally with restrictions. It says:
“Quantitation of BNP and NT-proBNP for the exclusion of a diagnosis of heart failure in patients presenting to a non-hospital setting to assist in decision-making regarding the clinical necessity of an echocardiogram where heart failure is suspected based on signs and symptoms but the diagnosis is uncertain.”
This test is only reimbursed by MBS once per patient in a 12-month period.
In other words, it is a useful test to perform to rule out heart failure (HF) so that the patient doesn’t have to be referred for an echocardiogram. If it is low <300ng/L (preferrably < 150ng/L), then HF is unlikely. Elevated levels may not confirm HF because there are other causes of elevated BNP or NT-pro-BNP but if the patient have symptoms or signs of HF, a referral is usually necessary.
References:
- Castiglione, V., Aimo, A., Vergaro, G. et al. Biomarkers for the diagnosis and management of heart failure. Heart Fail Rev 27, 625–643 (2022).
- https://www.rcpa.edu.au/Manuals/RCPA-Manual/Pathology-Tests/N/NT-pro-B-Natriuretic-peptide. Accessed 27th October 2024.
- https://www.rcpa.edu.au/Manuals/RCPA-Manual/Pathology-Tests/B/B-Type-natriuretic-peptide. Accessed 27th October 2024.
- 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure. Circulation. 2022;145:e876–e894.
