30th September 2018, Dr Chee L Khoo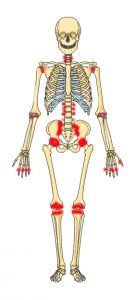
10-40% of patients with psoriasis have joint manifestations as part of a multi-system inflammatory disease (1). There is a strong association between psoriasis and elements of metabolic syndrome. Recent evidence suggests that patients with psoriasis have increased cardio-metabolic morbidity and mortality. Like other auto-immune collagen diseases, psoriatic arthropathy (PsA) often necessitate a referral to the specialists to manage the systemic and joint disease. The systemic and joint disease are managed by our rheumatology colleagues but who manages the cardio-metabolic risks?
The link between collagen disease is often bi-directional. Joint disability often reduces physical agility which often leads weight gain and its metabolic consequences. Side effects from drugs including corticosteroids add further insult to the metabolic derangement. Thus, insulin resistance, hypertension, impaired glucose tolerance or diabetes and dyslipidaemia are common conditions we see in patients with psoariasis. The chronic generalised inflammation provides the backdrop for linkage collagen diseases and metabolic syndrome. Chronic inflammation is associated with increased cardiovascular events.
There is strong evidence that patients with rheumatoid arthritis have an increased risk of cardiovascular morbidity and mortality probably related to the underlying generalised inflammation(2). Well, psoriatic arthropathy is also an inflammatory disease but the evidence relating to CV disease is less abundant.
Primary care data from the UK Clinical Practice Research Datalink (CPRD) containing 15 million individuals were analysed. Patients 18-89 years old with a diagnosis of psoriatic arthropathy between 1998-2014 were identified. The incidence of type 2 diabetes (T2D), cardiovascular disease (CVD), ischaemic heart disease (IHD) and peripheral vascular disease (PVD) in these patients were compared with two cohorts – the general population and patients with psoriasis but no arthropathy or other inflammatory arthritis. The results were published in the August issue of Rheumatology. There were some very significant findings relating to our role as GPs in managing patients with psoriasis.
PsA vs general population
The incidence of T2D was 40% higher in the PsA cohort. The incidence of any of the cardiovascular outcomes were 29% higher in the PsA cohort. Specifically, the incidence of IHD and PVD is 27% higher.
PsA vs psoriasis alone
The incidence of T2D was 53% higher in the PsA cohort. There were no difference in incidence of any cardiovascular outcomes, IHD and PVD between the PsA and psoriasis alone.
Which means, whether the joints are involved or not, the incidence of cardiovascular outcomes is increased if you have psoriasis. Once you have systemic and joint manifestations, the incidence of diabetes skyrockets.
This study have demonstrated an increased risk of T2D, IHD and PVD among patients with PsA compared with the general population, after adjustment for traditional risk factors. These results support the proposal in existing clinical guidelines that in order to reduce cardiovascular risk in patients with PsA, it is important to treat inflammatory disease as well as to screen and treat traditional risk factors early in the disease course.
The specialists manage the systemic and joint disease but as GPs, we have to screen and treat the cardiometabolic risk factors early in the disease. We are the specialists in managing cardio-metabolic risk.
Access the abstract here.
Reference:
- Ogdie A, Weiss P. The epidemiology of psoriatic arthritis. Rheum Dis Clin North Am 2015; 41:545–68
- Choy E, Ganeshalingam K, Semb AG, Szekanecz Z, Nurmohamed M. Cardiovascular risk in rheumatoid arthritis: recent advances in the understanding of the pivotal role of inflammation, risk predictors and the impact of treatment. Rheumatology 2014; 53:2143–
- Rachel CharltonAmelia Green Gavin Shaddick Julia Snowball Alison Nightingale William Tillett Catherine Smith Neil McHugh. Risk of type 2 diabetes and cardiovascular disease in an incident cohort of people with psoriatic arthritis: a population-based cohort study. Rheumatology Sept 2018
