14th April 2019, Dr Chee L Khoo
It’s difficult, isn’t it? Patients who are overweight or obese often has either significant cardiovascular risks or already have cardiovascular co-morbidities. These are the patients that need some assistance with weight loss but we always hesitate to prescribe Duromine®. We were taught and warned about the “dangers” of the drug especially in relation to “cardiovascular disease” and blood pressure. Is Duromine® effective in weight loss? Is it safe?
Duromine® (phentermine) is a psychostimulant drug of the substituted amphetamine chemical class, with pharmacology similar to amphetamine. We prescribe Duromine® as an appetite suppressant for short term use, as an adjunct to exercise and reducing calorie intake. On the Product Information (PI), there is a long list of contraindications which include
- pulmonary artery hypertension;
- existing heart valve abnormalities or heart murmurs;
- moderate to severe arterial hypertension;
- cerebro-vascular disease;
- severe cardiac disease including arrhythmias, advanced arteriosclerosis;
- concomitant treatment with Monoamine Oxidase (MAO) Inhibitors or within 14 days following their administration
All good to know but these are not our usual patients that we may consider Duromine®. There were no warnings about blood pressure or coronary heart disease in the PI, though. So, is it safe to use in overweight or obese patients who may have hidden atherosclerotic cardiovascular disease? Is it safe for patients with high blood pressure? Does it even effective for weight loss?
In a retrospective cohort study from electronic health records (EHRs) from several integrated health insurance and care-delivery systems in the United States were analysed. Records from adult health plan members 18 to 64 years old with a “first” phentermine fill (dose ≤ 37.5 mg/d) between January 1, 2010, and September 30, 2015 were included. They limited their study to members who had an BMI > 27 kg/m2 and excluded patients with a history of bariatric surgery or cancers. They analysed changes in body weight, BP and heart rate from baseline.
Effectiveness of Duromine®
They divided the patients into short-term, short-term intermittent, medium-term intermittent, medium-term continuous and long-term continuous where short-term was considered to be less than 3 months and medium-term to be less than 12 months.
At 6 months, short-term users lost 2.7% of weight. By 12 months, this had evaporated to only 1.4% weight loss and by 24 months, they return to their baseline weight. Short-term intermittent users had a little more weight loss (4.4% at 6 months) but suffered the same fate at 24 months – back to baseline.
Medium-term continuous and medium-term intermittent users fare a better losing 7.7% and 6.9% respectively at 6 months, 6.0% and 7.0% at 12 months respectively and 1.9% and 3.6% respectively at 24 months.
Long-term continuous users did the best with weight loss of 7.5% from baseline at 24 months.
Importantly, patients who responded early across all groups reached clinically significant levels of weight loss (≥ 5% on average) by 6 months and generally had more durable weight loss. Similar results from the literature on diet-induced weight loss, support the observation where early response tends to predict greater overall weight-loss success (1,2). This underscore the importance of not continuing to prescribe a medication to patients who do not appear to experience clinical benefit within 3 months.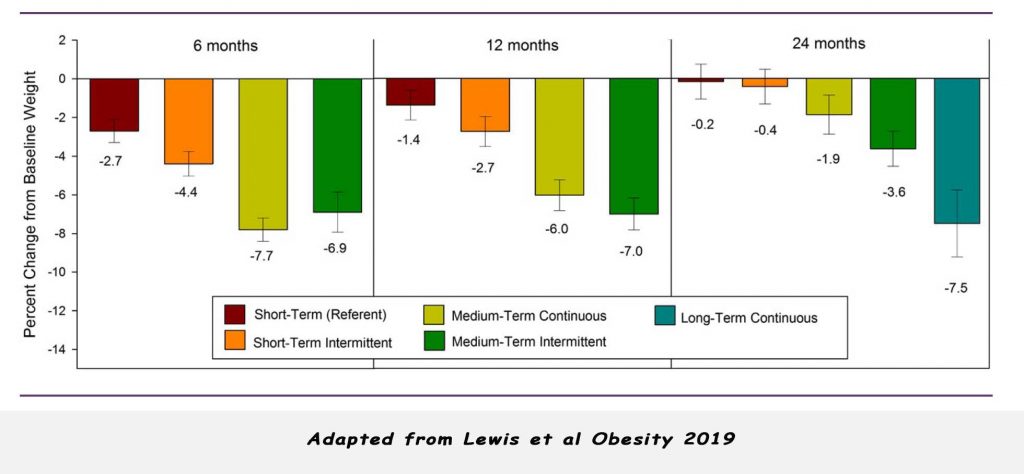
Safety of Duromine®
HR and BP
There was a slight increase in average heart rate amongst longer term users that normalised after discontinuation of phentermine. There was no change in heart rate with short-term users. Systolic BP was stable in short-term users at 6 and 12 months but increased by 1.8 mmHg at 24 months. BP in the other groups were actually lower than short term users. At 24 months, long term continuous users had -3.3 mmHg systolic BP compared with the other groups.
Cardiovascular safety
There was no increase in cardiovascular or death during 3 years use of Duromine®.
Limitations of this study
Naturally, the study include those that return as the drug is effective and not those that did not return because if wasn’t. The authors also acknowledged that physicians that prescribed longer-term phentermine are likely obesity specialists and their patients may have the benefit of participation of a comprehensive weight management program. Data for this study is sourced from outpatient facilities and may not have all hospitalisation events recorded.
Access this abstract here.
References:
- Miller CK, Nagaraja HN, Weinhold KR. Early weight-loss success identifies nonresponders after a lifestyle intervention in a worksite diabetes prevention trial. J Acad Nutr Diet 2015;115:1464-1471.
- Fabricatore AN, Wadden TA, Moore RH, Butryn ML, Heymsfield SB, Nguyen AM. Predictors of attrition and weight loss success: results from a randomized controlled trial. Behav Res Ther 2009;47:685-691.
- Kristina H. Lewis 1,2, Heidi Fischer3, Jamy Ard, et al. Safety and Effectiveness of Longer-Term Phentermine Use: Clinical Outcomes from an Electronic Health Record Cohort. Obesity (2019) 27, 591-602. doi:10.1002/oby.22430
