13th July 2019, Dr Chee L Khoo
First, it’s not good, then it’s Ok and now we are not sure. Maybe it is, maybe it isn’t. We are talking about eggs and the association with cardiovascular disease and mortality. It’s stuck in many of our and our patients’ minds that eggs are no good. It doesn’t help when the 2015-2020 Dietary Guidelines for Americans came out with somewhat contradictory recommendations: “ (1) Cholesterol is not a nutrient of concern for overconsumption” and (2) “Individuals should eat as little dietary cholesterol as possible while consuming a healthy eating pattern” (1). So, are eggs associated with an increase in cardiovascular disease and mortality or not?
Let’s not get confused about the message like many of my patients who came running in to see me when they heard it on current affairs somewhere. High blood cholesterol has been proven to be strongly associated with cardiovascular disease and mortality. Further, reducing cholesterol levels in these patients have been proven to reduce those numbers. What the American guidelines conclude is that the evidence linking dietary cholesterol with cardiovascular disease (CVD) is tenuous and therefore, they cannot draw meaningful conclusions linking dietary cholesterol and CVD.
The Lifetime Risk Pooling Project attempts to determine the associations of dietary cholesterol or egg consumption with incident CVD and all-cause mortality (2). Data from 6 cohort of patients, the Coronary Artery Risk Development in Young Adults (CARDIA) Study 13, Framingham Heart Study (FHS) 14 Framingham Offspring Study (FOS) 15, Jackson Heart Study (JHS) 16 and the Multi-Ethnic Study of Atherosclerosis (MESA) 17 were pooled and analysed (3-8). The primary outcomes were incident CVD and all-cause mortality. Incident CVD was a composite end point of fatal and nonfatal coronary heart disease (CHD), stroke, heart failure and CVD death from other causes. Secondary outcomes were CHD, stroke, heart failure, CVD mortality, and non-CVD mortality.
Overall, there were 29,615 participants with 524,376 person years of follow-up data. The median follow-up was 17.5 years. The 6 cohorts differed considerably in terms of sample size, age, sex, race/ethnicity, education level, BMI, and behavioural and clinical CVD risk factors, as well as incident CVD and all-cause mortality rates. Various modelling was used to identify any associations between dietary cholesterol or egg consumption and CVD and CV mortality adjusting for various confounding factors (e.g. BMI, diabetes, blood pressure, and serum lipids, dietary fats, animal protein, fibre, sodium, cholesterol-containing foods, or dietary patterns).
For each additional 300mg of dietary cholesterol consumed per day was significantly associated with higher risk of incident CVD but the increase was only modest – a relative increase of 17% but the adjusted absolute risk difference was only 3.24%. The all-cause mortality was increased by 18% with an adjusted absolute increase of 4.43%. With each additional half an egg consumed per day, there was 6% higher risk of incident CVD (adjusted absolute difference of 1.11%) and all-cause mortality increase of 8% (adjusted ARD of 1.93%) – see table below.
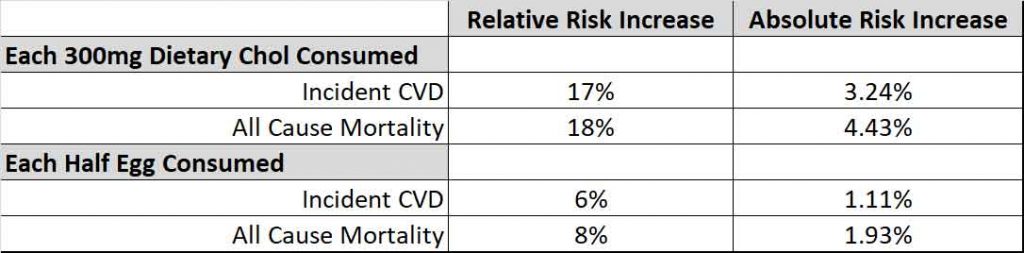
These associations remained significant after accounting for CVD risk factors, dietary fats, animal protein, fibre, sodium, or dietary patterns. However, the associations between dietary cholesterol consumption and incident CVD were no longer significant after adjusting for consumption of eggs, unprocessed red meat, and processed meat. The association between dietary cholesterol consumption and all-cause mortality was also no longer significant after adjusting for egg consumption. SO, it seems that egg consumption might be the major factor here.
Association with dietary cholesterol
When they analysed the subgroups of participants, association between dietary cholesterol consumption and incident CVD was stronger in participants with BMI lower than 25 compared with overweight or obese participants. The association was also stronger in participants without low (meaning high!) lipid levels, women and participants who consumed a high saturated fat diet.
Association with egg consumption
The association between egg consumption and incident CVD and all-cause mortality was also stronger in women and those without low lipid levels.
This is one of many studies (again) looking at the association between dietary cholesterol and egg consumption and CVD and all cause mortality. Trying to answer this simple question is going to be difficult. Cholesterol, saturated fat, and animal protein often coexist in foods. The interaction and independence between dietary cholesterol and these nutrients in relation to CVD and mortality remain uncertain. Data linking dietary cholesterol or eggs are sparse. Pretty much all the studies are observational studies. The study methodology and study population are heterogeneous and therefore difficult to analyse.
Egg consumption was commonly correlated with unhealthy behaviours such as low physical activity, current smoking, and unhealthy dietary patterns. Eggs and processed or unprocessed red meat are rich in other nutrients such as choline, iron, carnitine, and added sodium (for processed meat) that have been implicated in CVD risk via different pathways.
The effect of dietary cholesterol or egg consumption appears to be different in men and women, different depending on the lipid levels and whether there is consumption of other saturated fats.
References
- US Department of Health and Human Services and US Department of Agriculture. 2015-2020 Dietary Guidelines for Americans. 8th Edition. December 2015. https://health.gov/dietaryguidelines/2015/guidelines/
- Victor W. Zhong, Linda Van Horn, Marilyn C. Cornelis, et al. Associations of Dietary Cholesterol or Egg Consumption With Incident Cardiovascular Disease and Mortality. JAMA. 2019;321(11):1081-1095. doi:10.1001/jama.2019.1572
- The ARIC Investigators.The Atherosclerosis Risk in Communities (ARIC) study: design and objectives. Am J Epidemiol. 1989;129(4):687-702.
- Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41(11):1105-1116.
- Wong ND, Levy D. Legacy of the Framingham Heart Study: rationale, design, initial findings, and implications. Glob Heart. 2013;8(1):3-9.
- Feinleib M, Kannel WB, Garrison RJ, McNamara PM, Castelli WP. The Framingham Offspring Study: design and preliminary data. Prev Med. 1975;4(4): 518-525.
- Taylor HA Jr, Wilson JG, Jones DW, et al Toward resolution of cardiovascular health disparities in African Americans. Ethn Dis. 2005;15 (4)(suppl 6):4-17.
- Bild DE, Bluemke DA, Burke GL, et al. Multi-Ethnic Study of Atherosclerosis: objectives and design. Am J Epidemiol. 2002;156(9):871-881
