11th August 2019, Dr Chee L Khoo
All new anti-diabetic agents since 2008 have been mandated by the US FDA to conduct cardiovascular outcome trials (CVOT) to ensure that they are safe, or in statistical jargon, “non-inferior” to placebo in relation to major adverse cardiovascular events (MACE). 15 CVOTs assessing DPP‐4 inhibitors, GLP‐1 receptor agonists and SGLT‐2 inhibitors have been completed by the end of 2018 with several others to come yet. None of these trials reported an increase in risk for major adverse CV events (MACE). Surprise, surprise, six agents actually demonstrated CV benefits.
This has not only given us confidence in using these agents in patients with either established cardiovascular events or are at risk of developing events but has also spurred a major change in the treatment algorithm, “the what comes after metformin?” question.
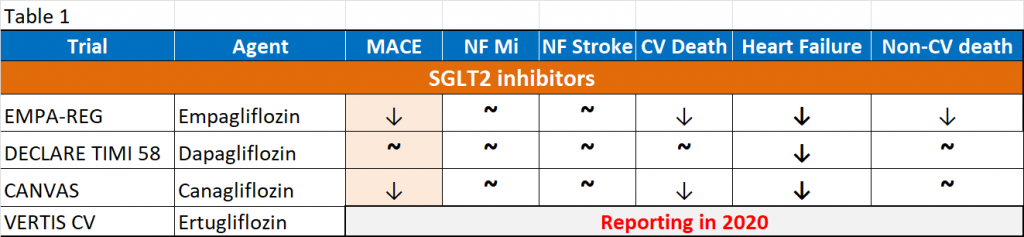
As more and more agents come to market with their CVOTs, it can become quite confusing when we try to decipher which agent is “better” than another in preventing certain cardiovascular events in certain subgroup of patients. You would have noted that the events in MACE lumped together non-fatal MI, non-fatal stroke and cardiovascular death. It’s a composite end point. Most of the trials were designed to show cardiovascular safety and may not be powered enough to show superiority over placebo. They are also not powered enough to show superiority of the individual components in the composite MACE. See Table 1.
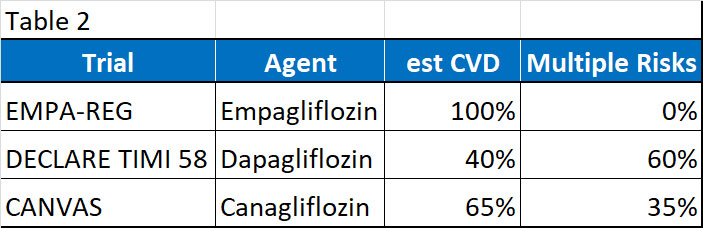
Further, Table 2 showed the breakdown of the trial population in EMPA-REG, DECLARE TIMI 58 and CANVAS. As you can see, both DECLARE TIMI 58 and CANVAS have a mixed of patients – some with established CVD and some with high cardiovascular risks. Both the CANVAS and DECLARE-TIMI 58 trials were not designed or powered to look at the patients with established CV disease and the high CV risk group separately.
All three agents consistently show reduction in hospitalisation for heart failure probably more in patients with established cardiovascular disease but again that is hypothetical. The other cardiovascular outcomes are less consistent. Although there is a reduction in non-fatal MI, there is no reduction in non-fatal stroke, suggesting that the effects are restricted to the heart (pump) and not atherosclerotic cardiovascular disease (ASCVD) (pipe).
GLP1-RA
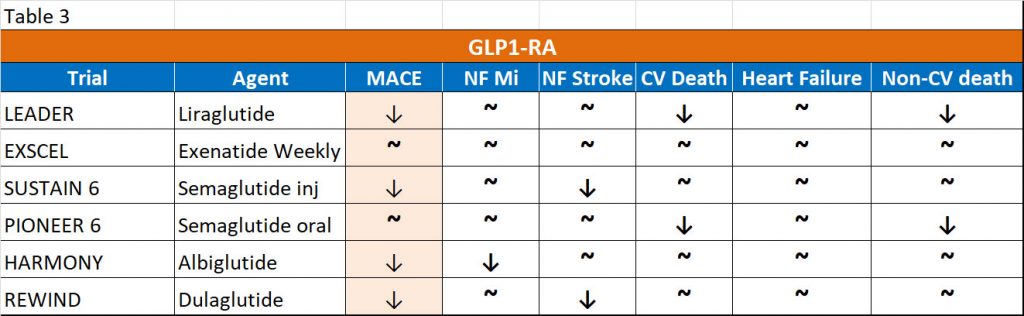
Similar “confusion” exists with CVOTs involving GLP1-RAs. Table 3 shows the CVOTs of different GLP1-RAs. All GLP1-RA CVOTs have shown a consistent reduction in the composite MACE with the studied drugs except Lixisenatide and Exenatide Weekly, which have shown neutrality. However, the driving force in the published data would suggest that these drugs have reduced MACE by either reduction of cardiovascular deaths (Liraglutide) or by reduction of myocardial infarctions (Albiglutide) or by reduction of non-fatal strokes (Semaglutide), a completely non-uniform finding, across the various GLP1-RA studied. Again, we are left confused as to whether GLP1-RA as a group produces these benefits or are the benefits individualised to the drugs. GLP1-RA have shown NO effect on hospitalisation for heart failure, an entity of increasing significance in patients of type 2 diabetes (T2D).
The evidence to dissect all these CVOTs is only slowly emerging and over the next few years, we will have to work with not quite evidence free zone but more like evidence incomplete zone. To make life more complicated, different studies have different patient populations, some with established cardiovascular diseases and some with only high-risk factors and the duration of the trials vary from <2 years to > 5 years. Thus, it’s not easy to compare apples with oranges.
For now, the next agent after metformin depends on whether the patient has either established CVD or CKD or not. If the answer is yes, you need a very good reason why this patient should not be on either an SGLT2 inhibitor or GLP1-RA.
References:
- Binayak Sinha and Samit Ghosal. Sodium-Glucose Cotransporter-2 Inhibitors (SGLT-2i) Reduce Hospitalization for Heart Failure Only and Have No Effect on Atherosclerotic Cardiovascular Events: A Meta-Analysis. Diabetes Ther (2019) 10:891–899
- Binayak Sinha and Samit Ghosal. Meta-analyses of the effects of DPP-4 inhibitors, SGLT2 inhibitors and GLP1 receptor analogues on cardiovascular death, myocardial infarction, stroke and hospitalization for heart failure. Diabetes Res Clin Pract. 2019 Apr;150:8-16
