10th September 2019. Dr Chee L Khoo
Have you noticed that most patients with type 1 diabetes (T1D) are not only small and petite but are often devoid of muscles when diagnosed. Insulin is a growth factor and without endogenous insulin, muscle growth is often stymied. We can’t push insulin therapy too hard because it will result in hypoglycaemia. Patients with T1D generally have normal lipids (especially triglycerides) and don’t have elements of metabolic syndrome. Well, that’s until they catch the obesogenic disease like everyone else in society.
We all know and see the diabesity epidemic before us. Just because you have T1D doesn’t protect you from the epidemic. Naturally, lifestyle issues including diet and physical activity (or lack of) are some of the main culprits to this epidemic. As the care of our patients with T1D improve over the decades, we are now looking after many patients with T1D who are in their 40s, 50s or even 60s. Like everyone else in the community, many of these patients are becoming obese and developing insulin resistance and its metabolic syndrome sequelae. These patients with T1D are also developing type 2 diabetes, the so-called double diabetes (DD).
The earliest description of DD dates back to 1991, when Teupe and Bergis demonstrated that individuals with T1D who had at least one relative with T2D had worse glycaemic control with increased insulin requirements and tended to have a greater body weight compared to those without a family history of T2D (1). Libman and Becker showed that features of DD can be present as early as 5 years of age, with full traits of insulin resistance and metabolic syndrome evident by the age of 14 years (2).
Should we be on a look out for these patients? Do these patients need different management strategies? It is important to identify these patients early as there is mounting evidence that patients with DD are at higher risk of developing future diabetes complications independent of their level of glycaemic control. However, there is still no clear criteria to define DD.
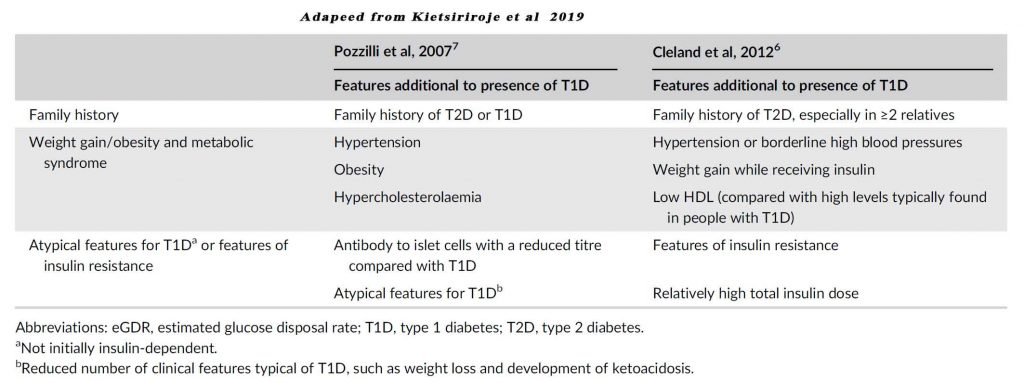
Some of the additional features that may suggest DD include;
- Family history of T2D especially in ≥2 relatives
- Hypertension
- Obesity
- Hyperlipidaemia (especially low HDL)
- Relative higher dose in insulin
- Other features of insulin resistance – fatty liver, skin tags, hyperuricaemia,
Merger et al conducted a cross-sectional study to measure the prevalence of comorbidities in DD by analysing data in the Diabetes-Patienten Verlaufsdokumentation registry from 392 specialized centres in Germany and Austria (3). Patients with DD had a rate of complications up to 3.5 times higher compared with people with T1D without metabolic syndrome who had identical HbA1c values. More worryingly, the rate of complications in the well-controlled DD subgroup was higher than in all those with T1D without metabolic syndrome regardless of glycaemic control.
In addition to an increased rate of complications, individuals with DD have a higher mortality rate. The hazard ratio for diabetes-related mortality from the FinnDiane study was significantly higher (adjusted hazard ratio of 2.52) in DD compared to T1D without metabolic syndrome (5)
It’s bad enough having diabetes (whether type 1 or type 2) but having both means having double the trouble. We need to manage not just the glycaemia and other metabolic parameters aggressively but we need to be on a look out for the increased complication rates in these patients.
Double diabetes means double jeopardy.
References
- Teupe B, Bergis K. Epidemiological evidence for “double diabetes”. Lancet. 1991;337:361-362.
- Libman IM, Becker DJ. Coexistence of type 1 and type 2 diabetes mellitus: “double” diabetes? Pediatr Diabetes. 2003;4:110-113.
- Merger SR, Kerner W, Stadler M, et al. Prevalence and comorbidities of double diabetes. Diabetes Res Clin Pract. 2016;119:48-56.
- Kietsiriroje N,Pearson S, Campbell M, Ariëns R, Ajjan R. Double diabetes: A distinct high-risk group? Diabetes Obes Metab. 2019;1–10
- Thorn LM, Forsblom C, Waden J, et al. Metabolic syndrome as a risk factor for cardiovascular disease, mortality, and progression of diabetic nephropathy in type 1 diabetes. Diabetes Care. 2009;32: 950-952.
- Cleland SJ. Cardiovascular risk in double diabetes mellitus–when two worlds collide. Nat Rev Endocrinol. 2012;8:476-485.
- Pozzilli P, Buzzetti R. A new expression of diabetes: double diabetes. Trends Endocrinol Metab. 2007;18:52-57.
