23rd November 2019, Dr Chee L Khoo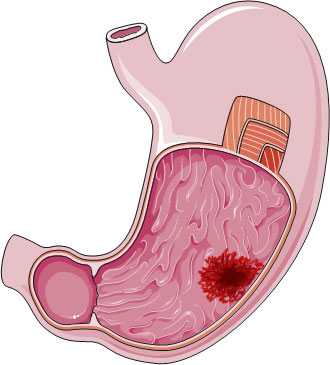
Treatment of helicobacter pylori infection (HPi) has been shown to reduce the incidence of gastric cancer (GC) worldwide (1,2). HPi may cause chronic inflammation which can lead to precancerous conditions. Since HPi is not always symptomatic and many patients may have untreated HPi for decades. Surely, if you have untreated HPi for decades, you might still be at risk of GC years down the track despite eradication of the infection. So, who amongst our treated patients are at future risk of GC despite eradication of HPI? Further, is there a point of no return whereby sufficient damage has been done and eradication of HPi no longer reduce the risk of GC?
GC is the third leading cause of cancer deaths worldwide causing an estimated >720,000 deaths per year globally (3). Approximately 50% of the global population is infected with helicobacter pylori (HP). 78% of GC are non-cardia gastric cancers and almost 90% of these are attributable to HP infection (4,5).
Pathophysiology
HP causes chronic gastric inflammation that can progress to the atrophic gastritis and intestinal metaplasia both of which are precancerous conditions. The risk of GC increases in relation to the severity and extent of those precancerous changes (6). Chronic HPi reduces gastric acid secretion (achlorhydria) and this contribute to gastric mucosal genetic instability (7). Achlorhydria is thought to promote the growth of gastric microbiome that processes dietary components into carcinogens (6).
However, not everyone with HPi will develop GC. Only a small subset of patients infected with HP develops significant gastro-duodenal pathology. Whether HPi causes diseases or not is mediated by an interplay between host, environmental and bacterial virulence factors. These virulence factors enable successful colonisation of the gastric mucosa and sustain persistent HPi, causing chronic inflammation and tissue damage, which may eventually lead to the development of peptic ulcers and gastric cancer.
Eradication of HP can result in resolution of gastric inflammation, halt the progression of gastric mucosal damage, prevent further HP induced DNA damage, improve gastric acid secretion, and restore the microbiome toward normal (7).
Does eradication of HPi reduce gastric cancers?
Controversies exist regarding whether eradication could still provide protection against GC once atrophic gastritis and/or intestinal metaplasia develops. Wong et al (2004) showed that eradicating HP reduced the incidence of GC only in subjects without premalignant gastric lesions, but not in those with atrophic gastritis, suggesting there might be a point of no return beyond which irreversible molecular changes renders eradication ineffective or less effective in preventing progression to cancer (8).
However, other RCTs have shown that amongst patients with atrophic gastritis and early GC, eradication of HPI reduce subsequent cancers (9). In a population-based mass eradication program on Matsu Island of Taiwan, H pylori eradication was shown to reduce the severity or reverse the presence of atrophic gastritis among subjects with premalignant gastric lesions at baseline and reduced gastric cancer incidence by 25%, from 40.3 to 30.4 per 100,000 person years (10). These later studies argue against the existence of a hard point of no return.
Is the risk of GC still there after eradication?
Take et al (2019) conducted a retrospective cohort study of 2737 patients in Japan who had yearly endoscopic follow-up after cure of HPi (11). They compared gastric cancer risk in the second decade of follow-up with that in the first decade. The mean follow-up period was 7.1 years but some were followed up for as long as 21.4 years. They found that the risk of developing diffuse-type gastric cancer became greater in the second decade of follow-up than during the first 10 years. This increase was only found in patients with mild-to-moderate gastric atrophy at baseline.
Another report of an analysis of a large database in Hong Kong described that a decrease in the risk of gastric cancer was more prominent more than 10 years after HP eradication therapy among people aged 40–59 years and even over 60 years (12).
In a retrospective cohort study collecting data from 371,813 veterans in the US, patients who had HPI detected and who developed GC subsequently, the cumulative incidence of cancer at 5, 10, and 20 years after detection of HPi was 0.37%, 0.5%, and 0.65%, respectively (13). Some of the factors associated with increased risk include older age at time of diagnosis of HPi, Asians, male and smokers. Patients that received treatment for HPi still had increased risk of GC but confirmed eradication have a reduced risk of GC.
What these studies suggest that eradication of HPi reduces the incidence of GC even in patients with significant precancerous changes on endoscopy. However, the risk is not zero despite eradication. Endoscopic surveillance of patients cured of HP should be continued beyond 10 years, even for those without severe atrophic gastritis.
References:
- Take S, Mizuno M, Ishiki K, et al. The effect of eradicating Helicobacter pylori on the development of gastric cancer in patients with peptic ulcer disease. Am J Gastroenterol. 2005;100:1037–42.
- Take S, Mizuno M, Ishiki K, et al. Seventeen-year effects of eradicating Helicobacter pylori on the prevention of gastric cancer in patients with peptic ulcer; a prospective cohort study. J Gastroenterol. 2015;50:638–44.
- IARC Helicobacter pylori Working Group. Helicobacter pylori Eradication as a Strategy for Gastric Cancer Prevention. Lyon, France: International Agency for Research on Cancer (IARC Working Group Reports, No. 8). Available at: http://www.iarc.fr/en/publications/pdfs-online/
- Schistosomes, liver flukes and Helicobacter pylori. IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Lyon, 7_14 June 1994. IARC Monogr Eval Carcinog Risks Hum 1994;61:1–241.
- de Martel C, Ferlay J, Franceschi S, et al. Global burden of cancers attributable to infections in 2008: a review and synthetic analysis. Lancet Oncol 2012; 13:607–615.
- Correa P. The biological model of gastric carcinogenesis. IARC Sci Publ 2004:301–310.
- Machado AM, Figueiredo C, Touati E, et al. Helicobacter pylori infection induces genetic instability of nuclear and mitochondrial DNA in gastric cells. Clin Cancer Res 2009;15:2995–3002.
- Wong BC, Lam SK, Wong WM, et al. Helicobacter pylori eradication to prevent gastric cancer in a high-risk region of China: a randomized controlled trial. JAMA 2004; 291:187–194.
- Fukase K, Kato M, Kikuchi S, et al. Effect of eradication of Helicobacter pylori on incidence of metachronous gastric carcinoma after endoscopic resection of early gastric cancer: an open-label, randomised controlled trial. Lancet 2008;372:392–397.
- Lee YC, Chen TH, Chiu HM, et al. The benefit of mass eradication of Helicobacter pylori infection: a community based study of gastric cancer prevention. Gut 2013; 62:676–682.
- Take, S., Mizuno, M., Ishiki, K. et al. J Gastroenterol (2019). https://doi.org/10.1007/s00535-019-01639-w
- Leung WK, Wong IOL, Cheung KS, et al. Effects of Helicobacter pylori treatment on incidence of gastric cancer in older individuals. Gastroenterology. 2018;155:67–75.
- Kumar S, Metz DC, Ellenberg S, Kaplan DE, Goldberg DS, Risk Factors and Incidence of Gastric Cancer After Detection of Helicobacter pylori Infection: A Large Cohort Study, Gastroenterology (2019). doi: https://doi.org/10.1053/j.gastro.2019.10.019
