
I told you last week that I am no expert and despite that I did write an article about the coronavirus. Well, I am doing that again this week but this time with a little more information and little bit more “expertise”. We have been getting oodles of feeds from many sources and I don’t know about you, but, all these bulletins really don’t help us working at the frontline. Sometimes, too many bulletins just confuses us with their recommendations. Other times, they are just pure useless updates. You end up pressing the DELETE button. This article is a report from the GP frontline.
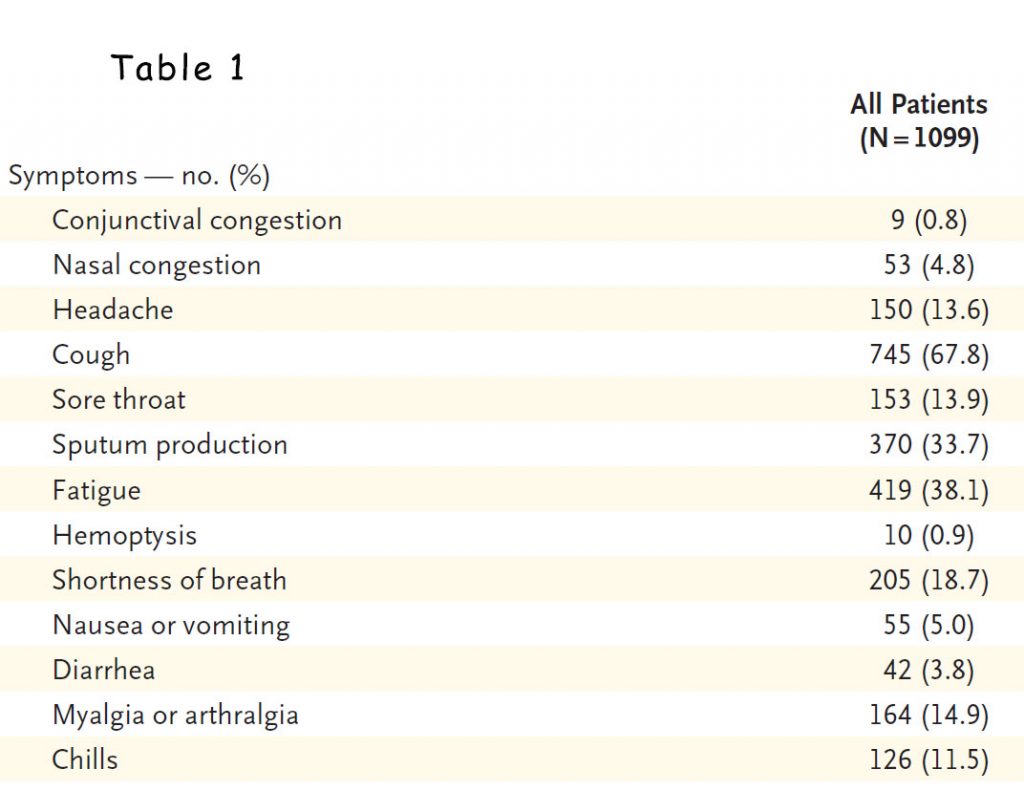
Let me first discuss the characteristic patient with the coronavirus infection and see whether this help us sort out the mess when we encounter patients in our practice with flu symptoms. Guan et al (Feb 2020) extracted data from 1099 patients admitted to 522 hospitals in 30 provinces in China which were confirmed by PCR nasal swab to have coronavirus, Covid 19, between Dec 11, 2019 and January 29, 2020 (1). They analysed the clinical characteristics of hospitalised patients infected with Covid-19.
These were patients admitted to hospital:
- Median age of patients was 47 years old
- ~40% females, ~60% males, 3.1% were health workers
- Mean incubation period was 4 days
- 5% admitted to ICU, 2.3% required ventilation, 1.4% died
- 88.7% had fever during hospitalisation (but only 43.8% had fever on admission)
- Only 27.3% had at least one co-exisitng illness (e.g. COPD, hypertension)
- 56.4% had the characteristic ground glass appearance on chest CT on admission
- 17.9% of non-severe disease and 2.9% of severe disease had normal chest CT
- Lymphopenia was present in 83.2% on admission
- Diarrhoea was uncommon (3%)
- Patients with severe disease were older than those with non severe disease by a median of 7 years
- Median hospital stay was 12 days
Now, remember, these are hospitalised patients diagnosed with Covid-19 and likely not represent the patients we see in primary care. Of note though, less than half had fever on admission. So, why do they insist that patients have to have fever before we consider swabbing them? Presenting symptoms from patients were quite minimal (see Table 1). Nothing more than the usual flu patients we see. “See your GP” is the national message. How can we tell without swabbing?
Coronavirus is just another flu, isn’t it? (the rest is just a media beat up)
One of the main fallacies amongst the non-believers is that coronavirus is just another flu and more people die from the flu each year, so, let’s get over it. Unfortunately, those views and beliefs encourage complacency. Inconsistent messages from our leaders perpetuate that complacency. I suspect this leads to delays in disaster planning in many countries including USA and Australia. We had 2-3 months since Wuhan told the world about the impending coronavirus pandemic but we appear to be only scrambling now to decide what to do to control the virus.
While the dreaded complication of influenza is pneumonia, that is usually bacterial pneumonia which is very treatable with antibiotics. Patients are usually in hospital for 5-7 days at the most. The “pneumonia” in coronavirus is an inflammatory pneumonitis, not a bacterial pneumonia. The pneumonitis is an inflammatory storm often referred to as a cytokine storm. A whole host of cytokines have been found to be increased in Covid-19 infections including IL1B, IFNγ, IP10, and MCP1. Obviously, our antibiotics have no role in treating this chemical pneumonitis. Thus far, not many agents have been successful in reducing this inflammatory storm including corticosteroids.
In a retrospective cohort multi-cohort study, all adult inpatients (≥18 years old) with laboratory-confirmed COVID-19 from Jinyintan Hospital and Wuhan Pulmonary Hospital (Wuhan, China) who had been discharged or had died by Jan 31, 2020 were studied. Out of 191 patients admitted to the two hospitals, 54 died in hospital. Of those who died, 48% had a co-morbidity including hypertension (30%), diabetes (19%), and coronary artery disease (8%). This means at least half the patients who died did not have a chronic illness – the type of patients we see in our practice and whom we are not swabbing.
In another single-centred, retrospective, observational study, 52 critically ill adult patients with SARS-CoV-2 pneumonia who were admitted to the intensive care unit (ICU) of Wuhan Jin Yin-tan hospital (Wuhan, China) between late December, 2019, and Jan 26, 2020 were studied. Of those that died (61.5%), most had organ function damage, including 35 (67%) with ARDS, 15 (29%) with acute kidney injury, 12 (23%) with cardiac injury, 15 (29%) with liver dysfunction, and one (2%) with pneumothorax. 37 (71%) patients required mechanical ventilation. Hospital-acquired infection occurred in seven (13·5%) patients. The average duration of hospitalisation is 3-4 weeks.
So, Covid-19 is not just a flu. Yes, older patients are more susceptible to severe disease but mortality is not exclusively in the elderly. Only one quarter of the patients admitted into hospital had a chronic illness which means three quarters are healthy young individuals (1). There is significant mortality in younger patients. Only half the patients that end up in hospital had a chronic illness. The rest are our usual patients in general practice.
By the time this article gets to you, the number of cases in Australia would have risen to >1000. Looking at many of the other countries’ graph, once the number of cases goes above 1000, the graph just takes off. Will they lock down the country when it gets to 1000? What about 4000 by next weekend? Will the government lock the country down then? Will they swab everyone then? What about 10,000? Will they do it then? What about 20,000? Or 50,000?
It generally takes 3-4 weeks after locking down before we see the numbers stabilise. If we lock down when we have 1000 cases, it will stabilise when we get to 40-50,000 cases. If we lock down when we get to 10,000 cases, it will be close to 250-300,000 before we stabilise. The economic costs are the same whenever they lock down but the cases will be exponential. Take your pick.
References:
Guan W, Ni Z, Hu Y et al. Clinical Characteristics of Coronavirus Disease 2019 in China. NEJM February 28, 2020 DOI: 10.1056/NEJMoa2002032
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study [published online ahead of print, 2020 Mar 11] . Lancet. 2020;S0140-6736(20)30566-3. doi:10.1016/S0140-6736(20)30566-3
Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study [published online ahead of print, 2020 Feb 24] [published correction appears in Lancet Respir Med. 2020 Feb 28;:]. Lancet Respir Med. 2020;S2213-2600(20)30079-5. doi:10.1016/S2213-2600(20)30079-5
