12th October 2020, Dr Chee L Khoo
We know from various diabetes prevention programs that intensive lifestyle interventions can be successful in reducing progression to diabetes. As GDM is more common in women with higher BMI and in the many high- risk groups and it is logical to ask the question “can we prevent GDM in these women?” If we could reduce progression of patients who has prediabetes to diabetes, we should, in theory, reduce prevalence of GDM in women who are at high risk of GDM. Could we apply those prevention principles in women at risk of GDM? It should be easier since most of these women would be more motivated.
The prevalence of gestational diabetes mellitus is increasing. 1:6 pregnancies is affected by diabetes and 85% of those are women with GDM. Internationally there are 16 million pregnancies with GDM each year. This represent a huge clinical and economic burden. Reducing the prevalence of GDM will have significant rewards both for the mother and future offspring health.
Interventions directed at preventing GDM could be dietary or exercise interventions, or a combination of these, dietary supplement interventions and pharmaceutical interventions. The dietary advice interventions for GDM prevention may be such as increasing fibre intake or aiming for a low glycaemic index diet. Others have included broader advice regarding “healthy eating” as part of more comprehensive lifestyle interventions.
Exercise or physical activity interventions for preventing GDM also varied from general advice to specific individualised programs using a range of different activities such as aerobic activities, stationary cycling or yoga. These have been employed in isolation or in combination with dietary interventions.
There have been many trials looking at prevention of GDM in different populations using different interventions at different stages of gestations. When you have so many trials with so many different populations and such a variety of interventions, one would need a meta-analysis or a systematic review. Indeed, in a recent overview of Cochrane reviews of interventions to prevent women from developing GDM, 11 previous Cochrane reviews comprising of 71 trials involving 23 154 women were the analysed.
Now, the headline summary of the overview says this: For dietary interventions alone, there were no proven benefit nor harm although the quality of evidence was poor. Similarly, for exercise interventions alone, there were also no proven benefit nor harm and the evidence was also graded as poor.
When diet and exercises were combined, there was possible benefit. The quality of evidence ranged from low to moderate. In particular, moderate-quality evidence in Shepherd 2017 indicated a possible benefit with reduction in the risk of GDM with combined diet and exercise interventions
during pregnancy compared with standard care (RR 0.85, 95% CI 0.71 to 1.01; 19 trials; 6633 women).
You would be forgiven to think that lifestyle measures, therefore, were not useful in preventing GDM. It’s a bit more complicated than that and we need to look into a bit detail in some of the studies quoted rather than depending on the executive summary of an overview of reviews of studies. Let’s look at just 4 of the studies (see Table 1 below).
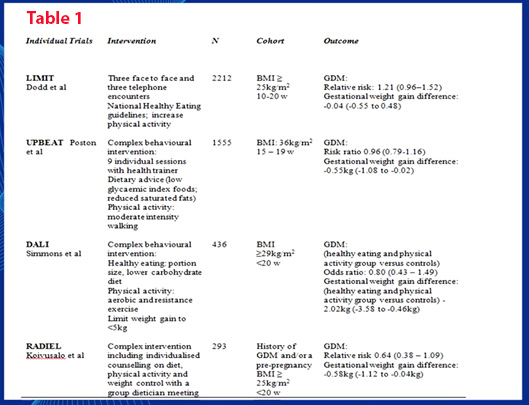
You can see that the different studies have different populations of women and commenced their intervention at different gestational age. Although the DALI study resulted in reduction of gestational weight gain (GWG), it did not reduce the prevalence of GDM. Yet the RADIEL study reduced GDM prevalence without reducing GWG. But their population was different.
What about interventions before conception?
Preconception and inter-conception interventions (between pregnancies). have been used, particularly in women at high risk of GDM, such as those who are overweight or obese (Yeung 2010), or with a history of GDM (Khan 2013; Shyam 2013). The opportunity exists to intervene with health promotion strategies prior to and between pregnancies for women identified with risk factors for GDM (Hanson 2015; Jack 1990). Song et al 2016) looked at 29 antenatal trials involving 11487 women interventions which started before 15 weeks reduced GDM by 22%.
What does all that mean in practice?
Well, you would think that lifestyle measures should make a difference but the evidence is very conflicting. There are other complicated issues which makes trials in GDM prevention difficult to compare. Which population are we studying? What is the ethnic mix of the study population? When were the interventions introduced? What were the diagnostic criteria for GDM? When were the women screened for GDM? What was the prevailing background prevalence of GDM in that population?
Obviously, we need more standardised study protocols. We probably need to begin our interventions pre-conception which means when the women are seeing their GP discussing their future plans, we should be discussing healthy lifestyles. It is an important conversation we need to have when we see women are overweight or obese or who are in one of those high risk groups for GDM.
References:
Griffith RJ, Alsweiler J, Moore AE, Brown S, Middleton P, Shepherd E, Crowther CA. Interventions to prevent women from developing gestational diabetes mellitus: an overview of Cochrane Reviews.
Cochrane Database of Systematic Reviews 2020, Issue 6. Art. No.: CD012394. DOI: 10.1002/14651858.CD012394.pub3.
