13th February 2021, Dr Chee L Khoo

Aspirin as a chemoprotective agent against colorectal cancer (CRC) has gone through quite exhaustive reviews over the last 20 years. After initially recommended against using aspirin for CRC prevention in 2007, the US Preventative Services Task Force (USPSTF) in 2015 recommended initiating low-dose aspirin use for the primary prevention of CVD and CRC in “adults aged 50 to 59 years who have a >10% 10-year CVD risk, are not at increased risk for bleeding, have a life expectancy of at least 10 years and are willing to take low-dose aspirin daily for at least 10 years” (1). Quite a lot of caveats for a recommendation, isn’t it? We better delve into why the caveats are there.
There is a bit of history to using aspirin for prevention of CRC. The role of aspirin in reducing the risk of CRC was stumbled upon by Kune GA et al back in 1988 (2). They examined 715 colorectal cancer cases and 727 age/sex-matched controls in data derived from a large, comprehensive, population-based study of this cancer conducted in Melbourne and found significant deficit among cases of hypertension, heart disease, stroke, chronic chest disease, and chronic arthritis. Now, these patients were likely to be on aspirin or non-aspirin NSAIDs for their cardiovascular disease or arthritis. And that may have reduced the incidence of CRC,
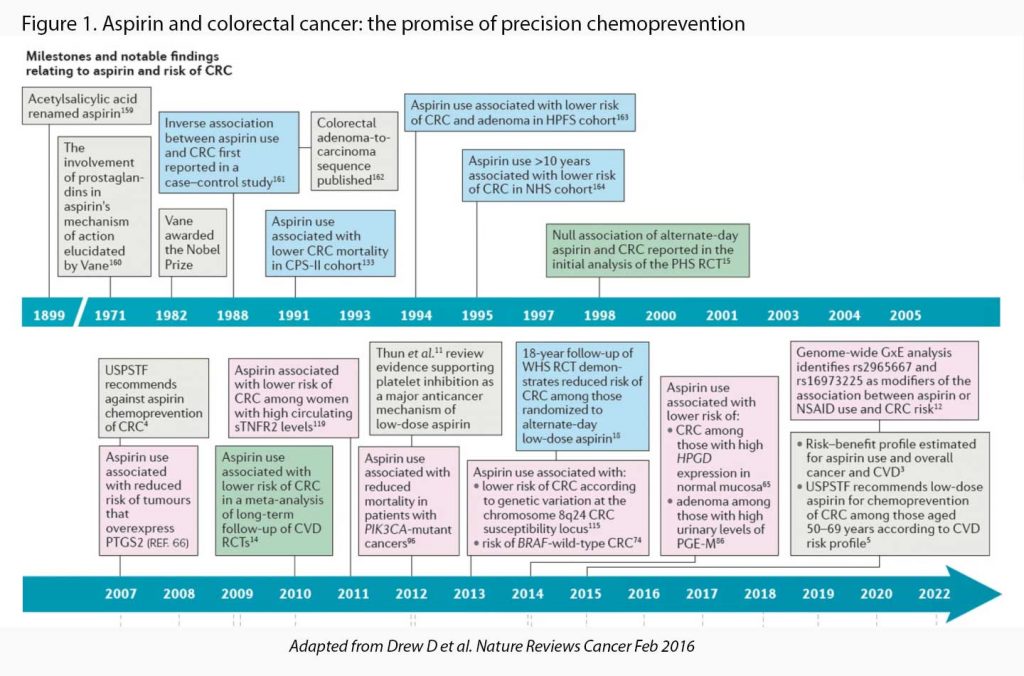
Several decades of research since then have provided considerable evidence demonstrating its potential for the prevention of cancer, particularly colorectal cancer. See Figure 1. It wasn’t all plain sailing, though. The Physicians’ Health Study (PHS), a placebo-controlled randomised controlled trial (RCT) of alternate-day 325 mg aspirin among 22,071 male physicians, found no association between aspirin use and CRC incidence over 12 years of follow-up (3). The Women’s Health Study (WHS), the largest placebo-controlled RCT of aspirin for primary prevention, compared alternate-day 100 mg aspirin with a median duration of treatment of 9 years (4). The results at completion of the originally planned follow-up of 10 years also provided no evidence of an effect of aspirin on CRC incidence.
Further, the Colorectal Adenoma/Carcinoma Prevention Programme 2 (CAPP2) trial observed no reduction in the risk of colorectal neoplasia among carriers of Lynch syndrome, a hereditary CRC syndrome, after 2.5 years of planned follow-up in those assigned to 600 mg of aspirin per day (5). A bit of a disappointment. It was a short duration study of a high-risk group.
However, when those RCTs were followed-up further, we saw more favourable evidence. For example, in the WHS, an inverse association between those randomised to aspirin and CRC incidence emerged 10 years after randomization (HR = 0.80 i.e. 20% reduction) (6). In the CAPP2 trial, a secondary pre-planned analysis, conducted after the first participant reached 10 years of follow-up, did show a significantly reduced risk of CRC in the per-protocol analysis (HR = 0.41 i.e. 59% reduction) (7).
More epidemiological evidence supporting the efficacy of aspirin for the prevention of cancer, especially CRC started to emerge. A recent pooled analysis of 10 cohort and case–control studies demonstrated that aspirin use was associated with a 29% reduction in the incidence of CRC (8) but primarily in those with single-nucleotide polymorphisms (SNPs).
More recently, a population-based study from Denmark reported that long-term, continuous use of low-dose aspirin and long-term use of non-aspirin NSAIDs were associated with a 27% reduced colorectal cancer risk. In this study, those who continuously used low-dose aspirin comprised only a small proportion of the low-dose aspirin users (9).
Just to throw a spanner in the works, in the Aspirin in Reducing Events in the Elderly (ASPREE) study, 19 114 relatively healthy adults aged 70 years or older (or 65 years or older for US racial/ethnic minorities) were randomised to either daily 100mg aspirin or placebo (10). Not only did aspirin use in healthy elderly persons not prolong disability-free survival over a period of 5 years but led to a higher rate of major haemorrhage than placebo. Higher all-cause mortality was also observed among apparently healthy older adults who received daily aspirin than among those who received placebo and was attributed primarily to cancer-related death. These results suggest a potential difference in the effect of aspirin at older ages. Note though, the vast majority of ASPREE participants (89%) had never used aspirin regularly before joining the study.
To look further into the role of aspirin in preventing CRC in older patients, Guo CG et al analysed pooled data from the NHS and HPFS with a total of 94 540 participants (11). Among individuals aged ≥70 years, regular use of aspirin was associated with a 20% lower risk of CRC compared with non-regular users which was consistent in both women and men. However, this inverse association was restricted to those who initiated regular use of aspirin before age 70 years.
In contrast, among those who did not regularly use aspirin before age 70 years, regular aspirin use at or after 70 years was not associated with reduced risk of CRC. The authors suggest that the initiation of aspirin use at an older age for the sole purpose of primary prevention of colorectal cancer should be discouraged; however, the findings support recommendations to continue using aspirin if initiated at a younger age.
At the beginning of my research into the role of aspirin for prevention of CRC, I thought it was all game, set and match in the conclusions. The evidence is not that overwhelming after all. The benefit appears to be in patients already taking it for cardiovascular protection. The evidence for the general population without CV risk is still limited and therefore needs to be personalised. Most of the participants who benefited were between 50-70 years old. The benefit for those over 70 years is only seen if aspirin were taken some years prior to 70 years.
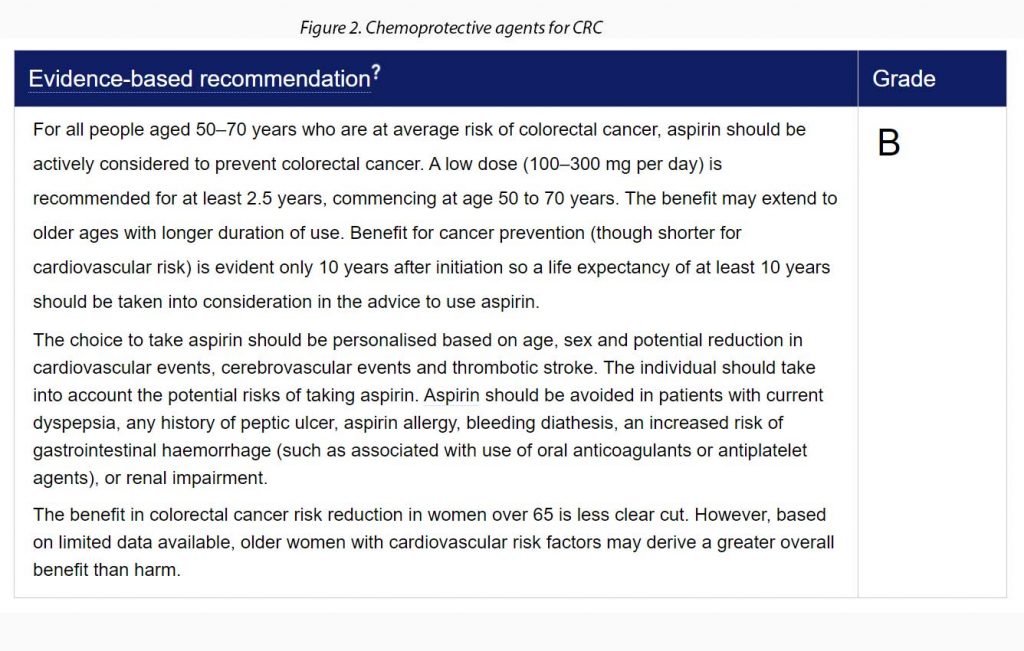
The Cancer Council of Australia’s colorectal cancer guidelines summarises the recommendations for average risk population and high-risk population here. See the brief version in Figure 2.
References:
- Bibbins-Domingo K; U.S. Preventive Services Task Force. Aspirin Use for the Primary Prevention of Cardiovascular Disease and Colorectal Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2016 Jun 21;164(12):836-45. doi: 10.7326/M16-0577. Epub 2016 Apr 12. PMID: 27064677.
- Kune, G. A., Kune, S. & Watson, L. F. Colorectal cancer risk, chronic illnesses, operations, and medications: case control results from the Melbourne Colorectal Cancer Study. Cancer Res. 48, 4399–4404 (1988)
- Sturmer, T. et al. Aspirin use and colorectal cancer: post-trial follow-up data from the Physicians’ Health Study. Ann. Intern. Med. 128, 713–720 (1998)
- Cook, N. R. et al. Low-dose aspirin in the primary prevention of cancer: the Women’s Health Study: a randomized controlled trial. JAMA 294, 47–55 (2005)
- Burn, J. et al. Effect of aspirin or resistant starch on colorectal neoplasia in the Lynch syndrome. N. Engl. J. Med. 359, 2567–2578 (2008)
- Cook, N. R., Lee, I. M., Zhang, S. M., Moorthy, M. V. & Buring, J. E. Alternate-day, low-dose aspirin and cancer risk: long-term observational follow-up of a randomized trial. Ann. Intern. Med. 159, 77–85 (2013)
- Burn, J. et al. Long-term effect of aspirin on cancer risk in carriers of hereditary colorectal cancer: an analysis from the CAPP2 randomized controlled trial. Lancet 378, 2081–2087 (2011)
- Nan, H. et al. Association of aspirin and NSAID use with risk of colorectal cancer according to genetic variants. JAMA 313, 1133–1142 (2015)
- Friis, S., Riis, A. H., Erichsen, R., Baron, J. A. & Sorensen, H. T. Low-dose aspirin or nonsteroidal anti-inflammatory drug use and colorectal cancer risk: a population-based, case-control study. Ann. Intern. Med. 163, 347–355 (2015)
- McNeil JJ, Nelson MR,Woods RL, et al; ASPREE Investigator Group. Effect of aspirin on all-cause mortality in the healthy elderly. N Engl J Med. 2018; 379(16):1519-1528. doi:10.1056/NEJMoa1803955
- Guo C, Ma W, Drew DA, et al. Aspirin Use and Risk of Colorectal Cancer Among Older Adults. JAMA Oncol. Published online January 21, 2021. doi:10.1001/jamaoncol.2020.7338
- https://wiki.cancer.org.au/australia/Clinical_question:Aspirin_for_prevention_of_colorectal_cancer#High-risk_population. Accessed 13th February 2021.
