2nd October 2021, Dr Chee L Khoo

We generally see two categories of patients with high lipids, one who had normal lipids earlier on in life but developed high lipids later in life because of modern living and one whose lipids were already high when they were young (and slim and fit). Most of the scientific studies linking high lipids with cardiovascular (CV) events look at lipid levels at a snap point in time, at enrolment and the follow up period just aren’t long enough. These participants are usually in the 40s and 50s. There must be a difference in CV risk in those who had a lifetime of high lipids compared with those who only have high lipids recently. So, is cumulative exposure to high lipids during young adulthood and middle age a stronger risk factor of future cardiovascular disease risk than high lipids at middle age?
We have data that informs us that elevated levels of LDL cholesterol in young adulthood were strongly and independently associated with later life coronary heart disease (CHD) in our analysis. Most studies are restricted in their baseline age to the 40-50 year-old probably because that’s when most CV events occur. Even fewer trials followed participants from young adulthood to later life. It has been challenging to elucidate independent contributions of risk factor exposures during early versus later adulthood because few trials measure both young adult exposures and substantial numbers of CV events, which primarily occur much later in life.
Domanski M et al (2020) used the data from the CARDIA study to assess the relationship of area under LDL-C versus age curve to incident CVD event risk to quantify the exposure duration risk (1). Incident CVD event risk depends on cumulative prior exposure to LDL-C and, independently, time course of area accumulation. The same area accumulated at a younger age, compared with older age, resulted in a greater risk increase, emphasising the importance of optimal LDL-C control starting early in life.
Navar-Boggan, AM. et al (2015) used the Framingham Offspring Cohort data to identify adults without incident cardiovascular disease to 55 years of age to explore the association between duration of moderate hyperlipidaemia (non–HDL cholesterol ≥ 4.15 mmol/L) in early adulthood and subsequent CHD (2). At median 15-year follow-up, CHD rates were significantly elevated among adults with prolonged hyperlipidaemia exposure by 55 years of age: 4.4% for those with no exposure, 8.1% for those with 1 to 10 years of exposure, and 16.5% for those with 11 to 20 years of exposure (P<0.001). This association persisted after adjustment for other cardiac risk factors including non–HDL cholesterol at 55 years of age (hazard ratio, 1.39 per decade of hyperlipidaemia).
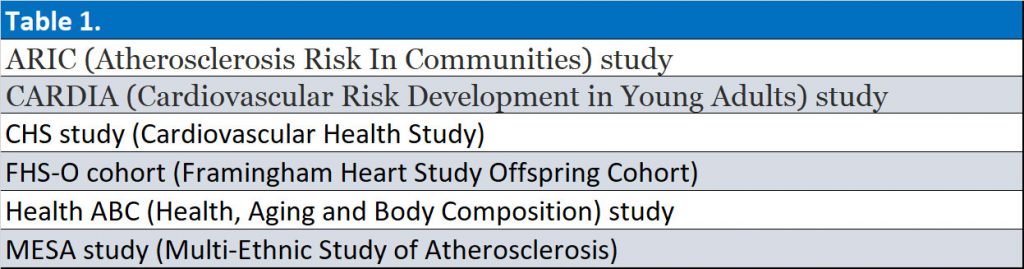
In an analysis of pooled data from 6 large prospective U.S. cohort studies (see Table 1), young adult exposures to elevated diastolic BP (DBP) and LDL-Cholesterol (LDL) were associated with incident CHD, and young adult exposure to elevated systolic BP (SBP) and DBP were associated with incident heart failure (HF), independent of later adult exposures (3). These findings concluded that exposures to elevated SBP, DBP, and LDL during young adulthood contribute independently to later life CHD and HF risks.
Zhang YY, et al. (2021) took this further by looking at time-weighted average (TWA) LDL-C, and the LDL-C slope change during young adulthood and middle age with incident CVD later in life (4). They analysed pooled data from 4 prospective cohort studies in the US (ARICS, CARDIA Study, FHS-O cohort and MESA). The study showed that cumulative LDL-C and TWA LDL-C during young adulthood and middle age were associated with the risk of incident CHD, independent of midlife LDL-C level. The hazard ratios were 1.57 (p= 0.01) for cumulative LDL-C, 1.60 (p< 0.001) for TWA LDL-C and 0.88 for LDL-C slope (p=0.28).
Exposure to high LDL levels during young adulthood is more likely driven by genetic determinants, and genetically determined LDL level is an important cause of atherosclerosis early in life; whereas later in life, atherosclerosis is likely driven by the same behavioural and environmental factors that affect the other risk factors included in the models (i.e., BP, diabetes, and smoking) (5-7).
As GPs, we are in a privileged position to be able to follow these patients over years. We know what their lipids were when they were “kids” or young adults and what their lipids are now. That is if we do check the lipids of young people which many of us don’t. These studies suggest that past levels of LDL-C may inform strategies for primary prevention of CHD and that maintaining optimal LDL-C levels at an earlier age may reduce the lifetime risk of developing atherosclerotic CVD.
The results of studies presented here both underscore the dependence of risk, not just on the present LDL-C level, but also the LDL-C versus time history, and offer a model to quantify the modulation of risk by the time course of LDL-C. Clinical trials of lowering LDL-C in young, even teenage, populations might show a major reduction in CVD incidence compared to risk reduction started later.
We are in a bit of a bind though. We don’t have data on treating young adults and their effect in reducing CV diseases later in life. According to current guidelines, to treat or not to treat patients with high LDL-C depends on what their CV risks are at that age. For most young adults, the CV risk will be <4% and current guidelines do not recommend commencing these patients on a statin. On the other hand, treating older adults with many years of cumulative LDL-C when they are older may not completely erase those elevated risks no matter how aggressive we treat these patients’ LDL-C.
We should also consider lifestyle intervention or statin treatment for adults with prolonged previous exposure to hyperlipidaemia. Current American Heart Association/American College of Cardiology cholesterol guideline recommends considering family history, C-reactive protein, coronary artery calcium, ankle brachial index, and lifetime CVD risk when making statin treatment recommendations.
References:
- Michael J. Domanski, Xin Tian, Colin O. Wu, et al. Time Course of LDL Cholesterol Exposure and Cardiovascular Disease Event Risk, Journal of the American College of Cardiology, Volume 76, Issue 13, 2020, Pages 1507-1516, ISSN 0735-1097, https://doi.org/10.1016/j.jacc.2020.07.059
- Navar-Boggan AM, Peterson ED, D’Agostino RB Sr, Neely B, Sniderman AD, Pencina MJ. Hyperlipidemia in early adulthood increases long-term risk of coronary heart disease. Circulation. 2015 Feb 3;131(5):451-8. doi: 10.1161/CIRCULATIONAHA.114.012477. Epub 2015 Jan 26. PMID: 25623155; PMCID: PMC4370230.
- Yiyi Zhang, Eric Vittinghoff, Mark J. Pletcher, et al. Associations of Blood Pressure and Cholesterol Levels During Young Adulthood With Later Cardiovascular Events, Journal of the American College of Cardiology, Volume 74, Issue 3, 2019, Pages 330-341, ISSN 0735-1097, https://doi.org/10.1016/j.jacc.2019.03.529.
- Zhang Y, Pletcher MJ, Vittinghoff E, Clemons AM, Jacobs DR Jr, Allen NB, Alonso A, Bellows BK, Oelsner EC, Zeki Al Hazzouri A, Kazi DS, de Ferranti SD, Moran AE. Association Between Cumulative Low-Density Lipoprotein Cholesterol Exposure During Young Adulthood and Middle Age and Risk of Cardiovascular Events. JAMA Cardiol. 2021 Sep 22. doi: 10.1001/jamacardio.2021.3508. Epub ahead of print. PMID: 34550307.
- S.J. Elder, A.H. Lichtenstein, A.G. Pittas, et al. Genetic and environmental influences on factors associated with cardiovascular disease and the metabolic syndrome. J Lipid Res, 50 (2009), pp. 1917-1926
- J. Cui, J.L. Hopper, S.B. Harrap. Genes and family environment explain correlations between blood pressure and body mass index Hypertension, 40 (2002), pp. 7-12
- J.N. Bodurtha, C.W. Chen, M. Mosteller, W.E. Nance, R.M. Schieken, J. Segrest. Genetic and environmental contributions to cholesterol and its subfractions in 11-year-old twins. The Medical College of Virginia Twin Study Arterioscler Thromb, 11 (1991), pp. 844-850
