29th November 2021, Dr Chee L Khoo
One of our biggest fears is missing an atrial fibrillation (AF) and patient is discharged from hospital following their first embolic stroke. Almost all the automatic sphygmomanometers do not check for cardiac rhythm and I make it a point to put a finger on the pulse each time to make sure patients are in sinus rhythm. You will remember not so long ago, Medicare decided that routine ECGs were not necessary and cut the rebates for performing and interpreting ECGs for GPs. There are tell-tale signs on the ECG or the Holter monitor that may suggest that AF is coming.
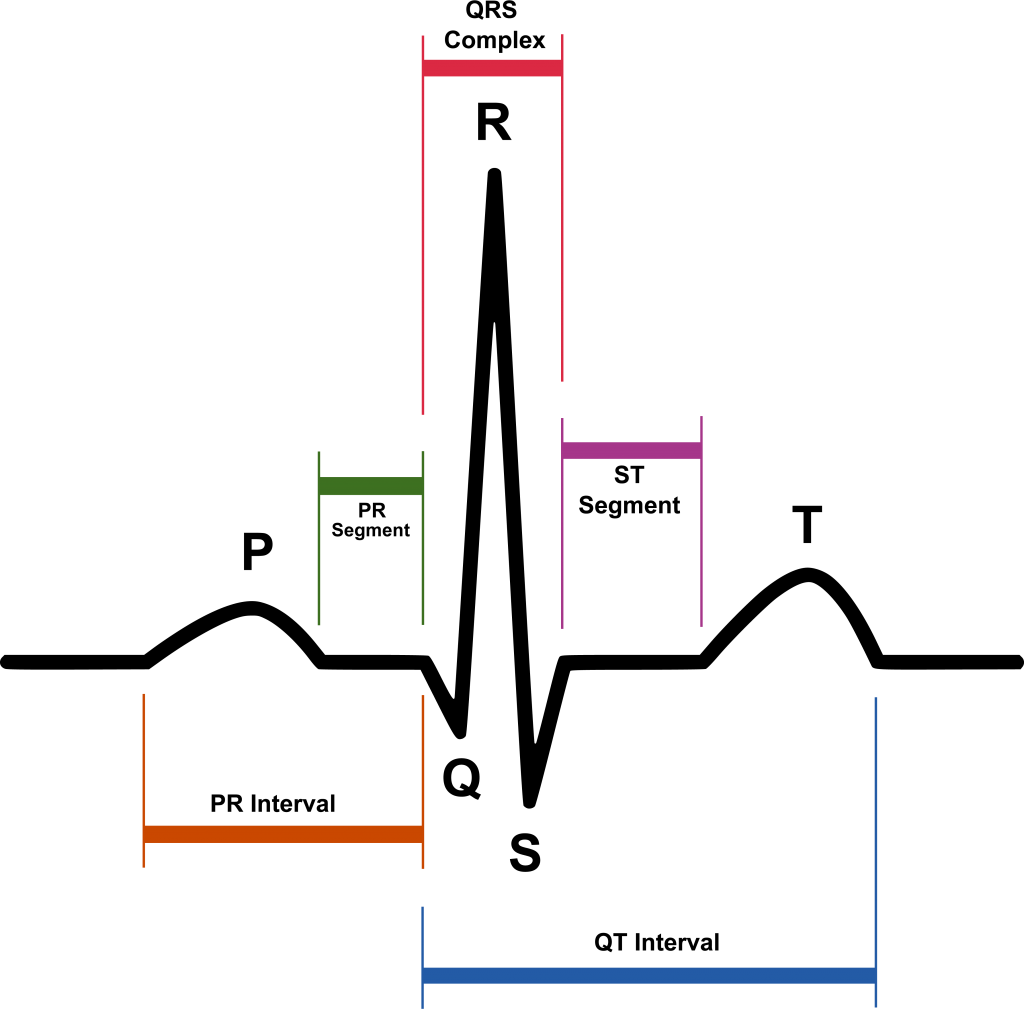
We know who are at higher risk of AF – patients with mitral valve disease, diabetes, existing heart failure, uncontrolled hypertension, thyroid disease, obesity, alcohol, smoking and sleep apnoea. The European Society of Cardiology’s guidelines define AF as an irregular heart rhythm without P waves lasting a minimum of 30 seconds. The time criterion is based on consensus [1]. Individuals with AF are at increased risk of stroke, dementia, heart failure and death. Thus, early diagnosis of AF and adequate treatment is important to prevent AF complications.
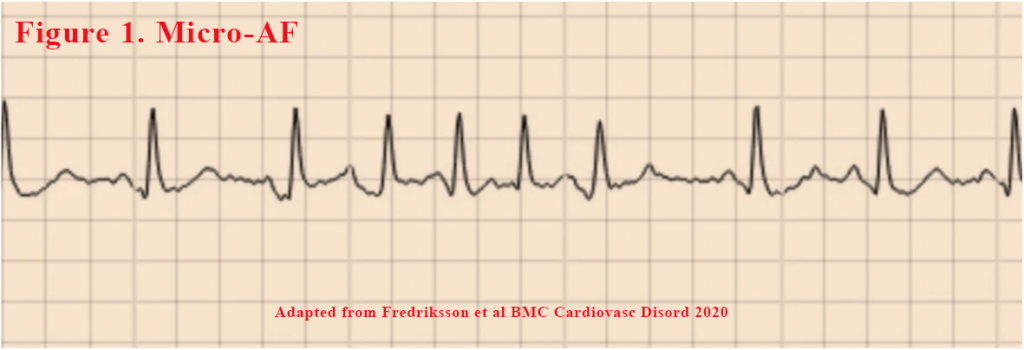
In clinical practice short episodes of AF-like activity is frequently detected during routine ECG or longer-term ECG monitoring. It has been shown that supraventricular ectopic beats (SVEBs) and supraventricular tachycardias (SVTs) are associated with increased risk of AF and stroke over time [2-8]. What about those shorter episodes of AF-like activity (so-called micro-AF). These are the short irregular SVTs, morphologically similar to AF, with absence of P waves (see Figure 1). These micro-AF has been shown to be more likely to progress into AF than short regular SVTs with or without P waves [15]. Should we treat these like we do with AF with anticoagulants? There are suggestions that perhaps, the existence of these micro-AF may indicate that AF is already present.
In a study by Binici et al., healthy individuals aged 55–75 years old underwent 48-h ECG monitoring, analysed for SVTs (≥20 beats) and ≥ 30 SVEBs per hour (2,3). After 6.3 years register follow-up, they were shown to have a 3-fold risk of AF and a 60% increased risk of stroke and death compared to controls. A linear association was seen between AF development and both frequency of SVEBs and length of SVTs [8]. Frequent isolated SVEBs and SVTs during 24-h ECG monitoring also predisposed for AF and stroke.
In a Swedish cohort study, individuals free from AF with a mean age of 64.5 years underwent 24-h ECG monitoring and were followed prospectively for > 13 years (9). SVTs with different characteristics were compared; irregular SVTs without P waves showed the strongest association with clinical AF, with a cumulative incidence of 47.4%. For irregular SVTs without P waves, a similar classification as our micro-AF definition was used.
In a recent study, STROKESTOP II, 28,712 Swedes aged 75 and 76 year were invited to a mass screening study (10). The study aimed to determine if short episodes of micro-AF, are not only a risk factor for future AF, but are also markers for already existing undetected AF.
All participants performed an index ECG using a 1-lead ambulatory handheld Zenicor II device. Those without a prior diagnosis of AF and NT-proBNP ≥125 ng/L were asked to perform intermittent 30 s ECG recordings four times daily for 2 weeks and to make extra recordings if palpitations occurred, using the same handheld Zenicor device. Participants without AF lasting at least 30 s (as per current definition) but with very short episodes of AF-like activity (micro-AF) during the intermittent ECG recordings in STROKESTOP II were invited to be part of this study.
Micro-AF was defined as an irregular tachycardia of sudden onset with episodes of ≥5 consecutive supraventricular beats without P waves lasting less than 30s. All participants with micro-AF and an unmatched control group free from AF were invited to undergo continuous ECG monitoring. The continuous monitor was a 1-lead event recorder, R-test 4 evolution.
13% of individuals with micro-AF seen during intermittent recordings already had AF detected by extended screening using continuous event recording. AF prevalence was found to be more than four times higher in the micro-AF group (13%) compared to the control group (3%).
The risk of stroke with paroxysmal AF is high even during sinus rhythm. Extensive atrial fibrosis has a role in the prothrombotic stage associated with AF but also isolates myocytes, creating an environment where re-entry arrhythmia, like AF, can exist. The presence of AF, SVTs and SVEBs may be indicative of atrial cardiomyopathy and might thereby be independently associated with an increase in stroke risk. Interestingly, in this study there were no significant increase in NT-proBNP level neither in individuals with micro-AF nor AF. The lack of significant increase could possibly be due to the low numbers of both micro-AF and AF in the study perhaps, the NT-proBNP cut-off level ≥ 125 ng/L may already be too high to detect smaller differences.
AF is a progressive disease which begins with short infrequent episodes and evolves to more permanent forms over time. Funny supraventricular or atrial abnormalities on the ECG or continuous ECG monitor may be red flags to either AF coming or AF already here. We have to pay a little more attention on the ECG and not to fully depend on the automated interpretation.
References:
- Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, Castella M, Diener HC, Heidbuchel H, Hendriks J, et al. ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. 2016;18(11):1609–78.
- Binici Z, Intzilakis T, Nielsen OW, Kober L, Sajadieh A. Excessive supraventricular ectopic activity and increased risk of atrial fibrillation and stroke. Circulation. 2010;121(17):1904–11.
- Johnson LS, Juhlin T, Juul-Moller S, Hedblad B, Nilsson PM, Engstrom G. A prospective study of supraventricular activity and incidence of atrial fibrillation. Heart Rhythm. 2015;12(9):1898–904.
- Engstrom G, Hedblad B, Juul-Moller S, Tyden P, Janzon L. Cardiac arrhythmias and stroke: increased risk in men with high frequency of atrial ectopic beats. Stroke. 2000;31(12):2925–9.
- Larsen BS, Kumarathurai P, Falkenberg J, Nielsen OW, Sajadieh A. Excessive atrial Ectopy and short atrial runs increase the risk of stroke beyond incident atrial fibrillation. J Am Coll Cardiol. 2015;66(3):232–41.
- Dewland TA, Vittinghoff E, Mandyam MC, Heckbert SR, Siscovick DS, Stein PK, Psaty BM, Sotoodehnia N, Gottdiener JS, Marcus GM. Atrial ectopy as a predictor of incident atrial fibrillation: a cohort study. Ann Intern Med. 2013;159(11):721–8.
- Murakoshi N, Xu D, Sairenchi T, Igarashi M, Irie F, Tomizawa T, Tada H, Sekiguchi Y, Yamagishi K, Iso H, et al. Prognostic impact of supraventricular premature complexes in community-based health checkups: the Ibaraki prefectural health study. Eur Heart J. 2015;36(3):170–8.
- Kochhauser S, Dechering DG, Dittrich R, Reinke F, Ritter MA, Ramtin S, Duning T, Frommeyer G, Eckardt L. Supraventricular premature beats and short atrial runs predict atrial fibrillation in continuously monitored patients with cryptogenic stroke. Stroke. 2014;45(3):884–6.
- Johnson LSB, Persson AP, Wollmer P, Juul-Moller S, Juhlin T, Engstrom G. Irregularity and lack of p waves in short tachycardia episodes predict atrial fibrillation and ischemic stroke. Heart Rhythm. 2018;15(6):805–811.
- Fredriksson, T., Gudmundsdottir, K.K., Frykman, V. et al. Brief episodes of rapid irregular atrial activity (micro-AF) are a risk marker for atrial fibrillation: a prospective cohort study. BMC Cardiovasc Disord 20, 167 (2020). https://doi.org/10.1186/s12872-020-01453-w
