22nd May 2022, Dr Chee L Khoo
The close association of inflammation and cardiovascular disease is well known for some time. Inflammation is an essential mediator of all stages of atherosclerosis, from initiation to progression and the development of thrombotic complications (1,2). Circulating immune cells play a critical role in the build-up of atherosclerotic plaques by adhering to activated endothelium and infiltrating the arterial wall to become lesional cells (3). So, where do all these inflammatory cells come from?
After an acute cardiovascular event, in response to sympathetic signalling, the bone marrow (BM) is activated. This leads to triggering of an increased haematopoiesis and the release of progenitor cells that activate spleen production of monocytes. This actually leads to aggravation of the atherosclerosis progression (4-7). So, we know that inflammation is associated with atherosclerosis. Other chronic conditions are also also associated with inflammation. Diabetes mellitus and obesity are associated with increased circulating neutrophils and monocytes. In humans, it has been suggested that chronic stress accelerates haematopoiesis, giving rise to higher levels of inflammatory cells that might contribute to the atherosclerotic process.
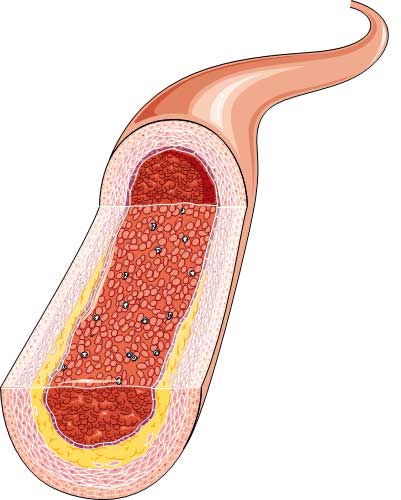
The bone marrow (BM) is the primary site of haematopoiesis, and the proliferation and migration of haematopoietic progenitors are regulated by various physiological and pathological stimuli. We can assume that the circulating progenitor cells originated from the bone marrow. Are we able to detect early levels of bone marrow activation before the markers of inflammation are detected?
High metabolic activity can be detected by imaging techniques such as 18F-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) imaging. This technique has been used to characterise BM activation after acute coronary syndrome based on a higher 18F-FDG uptake related to an increased glucose consumption due to cellular proliferation, and vascular inflammation which correlates with macrophage density as measured by histology and immunohistochemistry.
Ana Devesa et al studied BM activation in apparently healthy middle-aged individuals and explored its association with cardiovascular risk factors and subclinical atherosclerosis (8). The study population consisted of participants in the Progression of Early Subclinical Atherosclerosis (PESA) study cohort. PESA is an observational prospective cohort study of 4184 asymptomatic employees at Santander Bank in Madrid. Participants are excluded if they had previous CVD, CKD or morbid obesity.
At enrolment, fasting blood biochemisty and inflammatory makers were collected. Metabolic syndrome (MetS) was defined if participants had at least 3 of central obesity, elevated triglycerides, low HDL, elevated glucose and hypertension. 6 vascular territories were analysed by MRI. The presence, number and plaque volumes were defined for each territory. Lumbar vertebra L3 and L4 were analysed with 18F-FDG PET/MRI as a marker of bone marrow activation.
Results
946 participants underwent whole body 18F-FDG PET/MRI. Compared with participants without bone marrow activation, participants with bone marrow activation were more likely to have MetS , central obesity, hypertension, higher TG, lower HDL-C, higher glucose, HbA1c and insulin resistance (as measured by HOMA-IR). Bone marrow activation is also associated with higher numbers of leucocytes especially neutrophils and red cells, CRP, ferritin and fibrinogen.
Arterial 18F-FDG uptake is a surrogate for high vascular metabolic activity due to macrophage accumulation, the precursor of atherosclerosis. Participants with bone marrow activation were more likely to have vascular 18F-FDG uptake, more sites of uptake and higher degree of uptake. Subjects with BM activation plus vascular 18F-FDG uptake had a higher prevalence of plaques than those with BM activation but without vascular 18F-FDG uptake. The BM activation plus vascular 18F-FDG uptake group had more plaques (4 vs. 2, P<0.001) and a higher plaque burden. This association was consistent when atherosclerosis was evaluated by 2D and 3D vascular ultrasound; subjects with BM activation plus 18F-FDG uptake had a higher prevalence and number of plaques and higher plaque burden when compared with those with BM activation but without vascular uptake.
In a subgroup of participants without systemic inflammation, the association between bone marrow activation and MetS was still present.
In summary, this study not only demonstrates that bone marrow activation is associated with metabolic syndrome and its elements as well as arterial plaques, but that association is maintained even in the absence of systemic inflammatory markers. Further, bone marrow activation contributes to early atherosclerosis by increasing the inflammatory cell proliferation.
In our patients who have early signs of elements of the metabolic syndrome forming, the arterial atherosclerosis may well be underway. As their physician, we need to double up in our efforts to unwind the clock to stop these patients being a statistic.
References:
1. Libby P, Loscalzo J, Ridker PM, Farkouh ME, Hsue PY, Fuster V, et al. Inflammation, immunity, and infection in atherothrombosis: JACC review topic of the week. J Am Coll Cardiol 2018;72:2071–2081.
2. Poller WC, Nahrendorf M, Swirski FK. Hematopoiesis and cardiovascular disease. Circ Res 2020;126:1061–1085.
3. Swirski FK, Libby P, Aikawa E, Alcaide P, Luscinskas FW, Weissleder R, et al. Ly-6Chi monocytes dominate hypercholesterolemia-associated monocytosis and give rise to macrophages in atheromata. J Clin Invest 2007;117:195–205.
4. Dutta P, Courties G, Wei Y, Leuschner F, Gorbatov R, Robbins C, et al. Myocardial infarction accelerates atherosclerosis. Nature 2012;487:325–329.
5. Cremer S, Schloss M, Vinegoni C, Brody F, Zhang S, Rohde D, et al. Diminished reactive hematopoiesis and cardiac inflammation in a mouse model of recurrent myocardial infarction. J Am Coll Cardiol 2020;75:901–915.
6. Courties G, Herisson F, Sager HB, Heidt T, Ye Y, Wei Y, et al. Ischemic stroke activates hematopoietic bone marrow stem cells. Circ Res 2015;116:407–417.
7. Courties G, Frodermann V, Honold L, Zheng Y, Herisson F, Schloss MJ, et al. Glucocorticoids regulate bone marrow B lymphopoiesis after stroke. Circ Res 2019;124:1372–1385.
8. Devesa A, Lobo-González M, Martínez-Milla J, Oliva B, García-Lunar I, Mastrangelo A, España S, Sanz J, Mendiguren JM, Bueno H, Fuster JJ, Andrés V, Fernández-Ortiz A, Sancho D, Fernández-Friera L, Sanchez-Gonzalez J, Rossello X, Ibanez B, Fuster V. Bone marrow activation in response to metabolic syndrome and early atherosclerosis. Eur Heart J. 2022 May 14;43(19):1809-1828. doi: 10.1093/eurheartj/ehac102. Epub 2022 Mar 11. PMID: 35567559; PMCID: PMC9113301.
