24th November 2022, Dr Chee L Khoo

One of the problems in primary care in trying to keep up to date is that 1) there is just so many guidelines we need to keep track of 2) we don’t when the new guidelines are updated. It is often mentioned that, on average, it takes 16 years when guidelines are published before it lands on our desk and be adopted in practice. Pretty sad really. Well, here at GPVoice, we try to keep you up to date. Did you know there has been an update to the RACGP Diabetes Management Guidelines? Is it very different from the last update in 2020? Can you spot the difference?
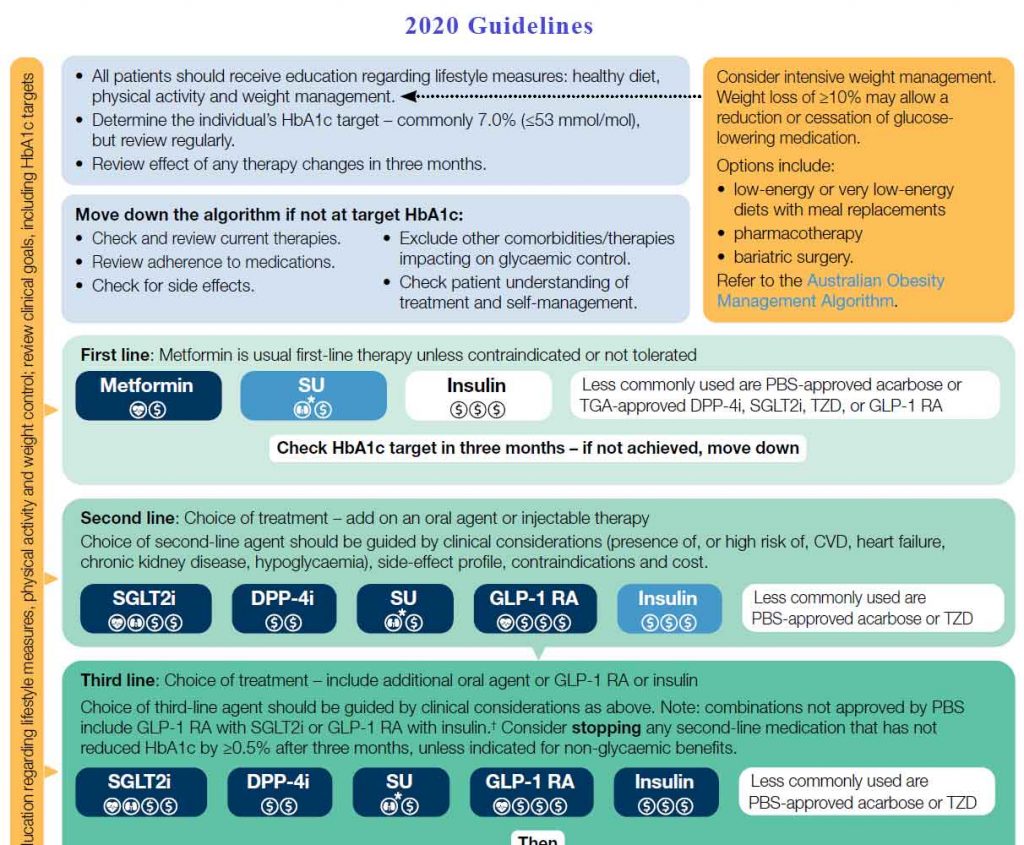
This is the last guideline in 2020 (1):
This is the current guideline released in August 2022 (2):
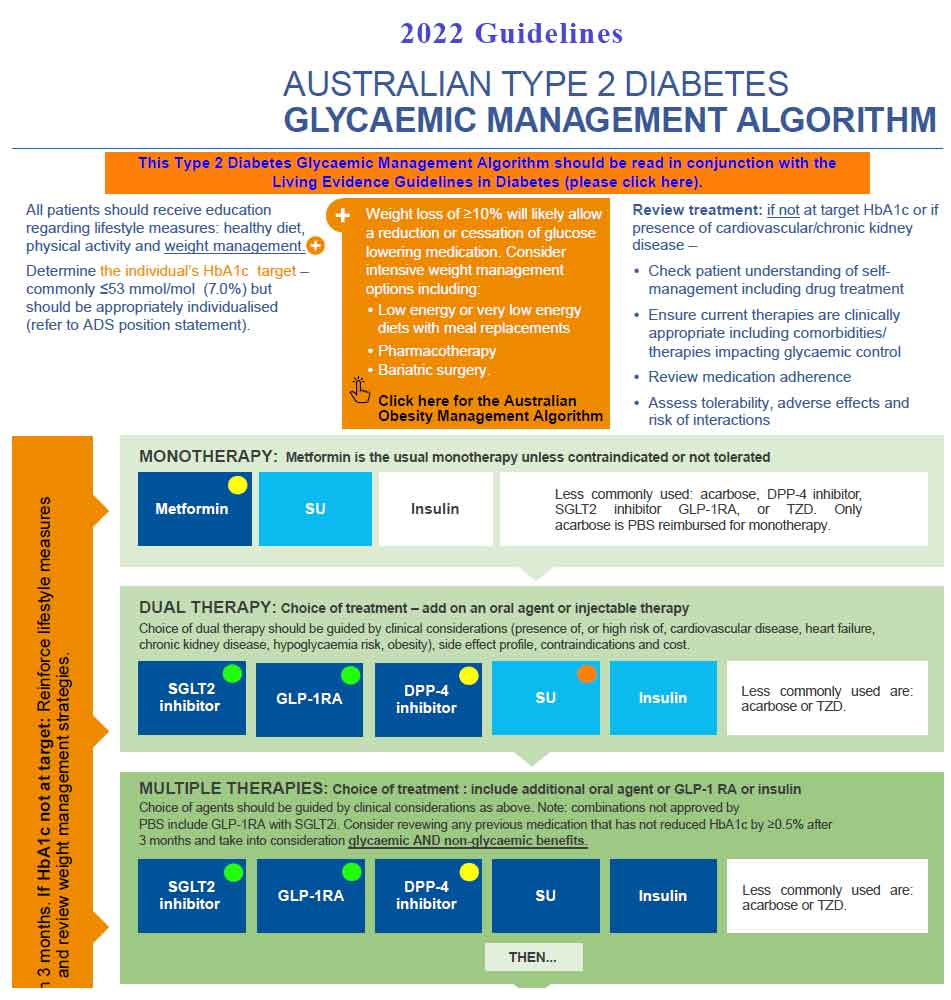
I don’t know about you but they look pretty much the same to me albeit with some font and colour changes. It’s almost an exercise in “Where is Wally?” Let’s unpack what has and what hasn’t changed.
Instead of the non-specific recommendations to use an SGLT2 inhibitor or GLP1-Receptor Antagonists in patients with high risk of or has established CVD or CKD in the previous guidelines, the new recommendations are a bit more specific. It now says “Recommendation for addition of an SGLT2i (or GLP-1RA where SGLT2i is not tolerated or contraindicated) to other glucose lowering medication(s) in adults with type 2 diabetes who also have cardiovascular disease, multiple cardiovascular risk factors and/or kidney disease” in green in the SGLT2i and GLP-1RA boxes. If you blink, you might miss the change!

However, what has also changed is the box which reminds us of weight management and is now in bright orange right in the middle of the top part of the algorithm. The message remains the same. Weight loss of >10% will likely allow a reduction or cessation of glucose lowering medication. It reminds us to consider low energy or very low energy diets with meal replacements.
The original DiRECT trial was done under real-life, primary care conditions. 306 individuals with T2D diagnosed in the preceding 6 years were recruited from 46 general practices from Scotland and the Tyneside region of England (3,4). The DiRECT trial have shown that it is possible to achieve significant weight loss of 10-15 kg of body weight and diabetes remission with dietary and lifestyle intervention in a primary care setting.
My colleagues and I conducted an audit on 51 patients in my practice who has type 2 diabetes and who was offered a low carbohydrate diet over three months. 34 patients completed the three months of diet and 24 months of data was available for audit. Over the subsequent 21months, patients were encouraged to follow a reduced calorie diet with a particular emphasis on lowering carbohydrate intake. Data were analysed and literature search was conducted with enormous assistance from Drs Ritesh Chimoriya, Milan Piya and Prof David Simmons.
The 12 months and 24 months results of the audit were presented at the Australian Diabetes Society meeting in 2019 and 2020. Thanks to my colleagues, the paper is now published in the Australian Journal of Primary Health (5). In essence, we found that compared to baseline, the average weight loss at 12 and 24months was 7.1±7.0kg (102.2±20.9kg vs 95.1±18.7kg, P<0.001) and 4.2±7.7kg (102.2±20.9kg vs 98.0±18.2kg, P=0.003), respectively. Haemoglobin A1c (HbA1c) was significantly reduced at 12months (6.9±1.5% vs 6.3±0.9%, P=0.003), but not at 24months. Over half of the participants achieved HbA1c <6.5% at 12 and 24 months, and one-third met the criteria for diabetes remission at 24 months.
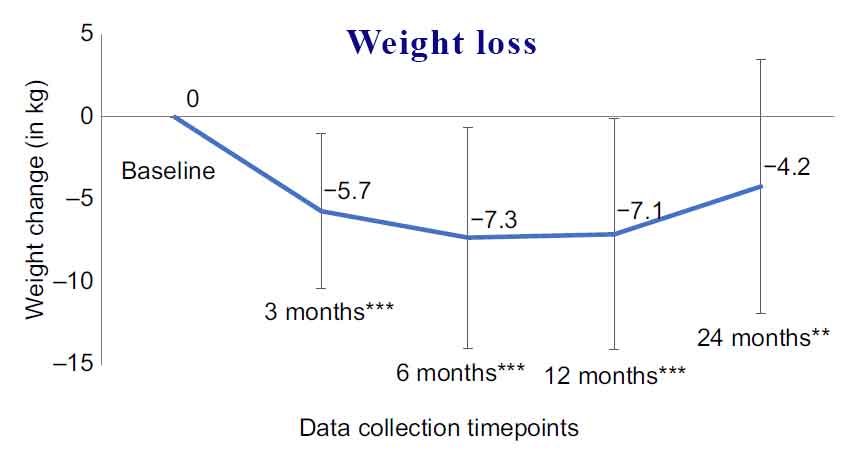
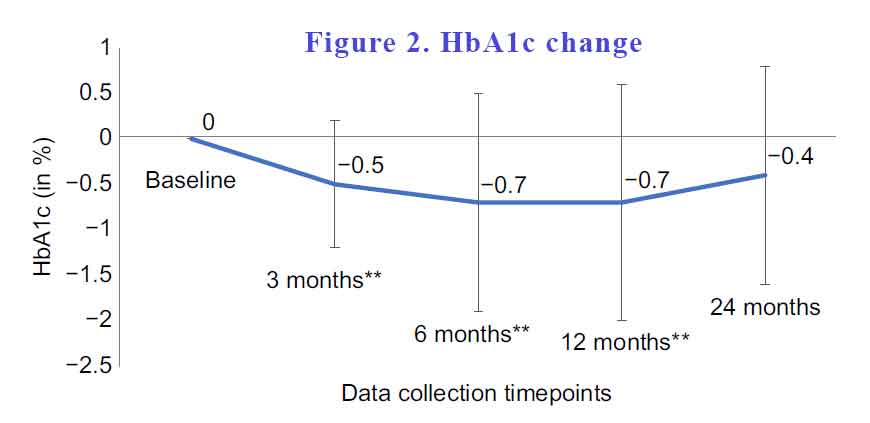
This study demonstrated the effectiveness of a dietary intervention program offered in primary care by a GP as part of routine diabetes care. Irrespective of T2D duration, this study found that significant weight loss can be achieved and that most patients with T2D and who are overweight or obese were able to follow a partial meal replacement plan with minimal support, and simple advice from a GP. The dietary intervention can be successfully replicated in an Australian primary care setting as it does not require any additional support, or a special setup.
The dietary intervention is easy to adapt as it can be carried out by a single practitioner. If rolled out, this partial meal replacement intervention in general practice would certainly improve the outcomes of people with T2D and also potentially reduce the burden on secondary and tertiary care diabetes services locally, that are under stress (Thakur et al. 2021) (6).
You can view the abstract here.
DOMTRU in conjunction with the George Institute for Global Health, Faculty of Medicine, University of New South Wales and a few other universities is honoured to be part of a randomised controlled trial of medically tailored meals (MTM) in participants with T2D with HbA1c ≥ 8% who experience difficulties accessing and/or preparing nutritious food.
If you have patients that fit the above criteria, you can enrol them in the trial. Your practice will benefit from learning from offering a dietary option as part of the management of your patients with T2D in accordance to current management guidelines. Here is the full description of the trial and the process of recruitment.
References:
- https://www.racgp.org.au/clinical-resources/clinical-guidelines/key-racgp-guidelines/view-all-racgp-guidelines/diabetes/type-2-diabetes-goals-for-optimum-management
- https://www.racgp.org.au/getattachment/2938847a-968c-40bc-b147-df2d651ab508/Australian-type-2-diabetes-management-algorithm.pdf.aspx
- Lean MEJ, Leslie WS, Barnes AC, Brosnahan N, Thom G, McCombie L, Peters C, Zhyzhneuskaya S, Al-Mrabeh A, Hollingsworth KG, Rodrigues AM, Rehackova L, Adamson AJ, Sniehotta FF, Mathers JC, Ross HM, McIlvenna Y, Stefanetti R, Trenell M, Welsh P, Kean S, Ford I, McConnachie A, Sattar N, Taylor R (2018) Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. The Lancet 391, 541–551. doi:10.1016/S0140-6736(17)33102-1
- Lean MEJ, Leslie WS, Barnes AC, Brosnahan N, Thom G, McCombie L, Peters C, Zhyzhneuskaya S, Al-Mrabeh A, Hollingsworth KG, Rodrigues AM, Rehackova L, Adamson AJ, Sniehotta FF, Mathers JC, Ross HM, McIlvenna Y, Welsh P, Kean S, Ford I, McConnachie A, Messow C-M, Sattar N, Taylor R (2019) Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes & Endocrinology 7, 344–355. doi:10.1016/S22138587(19)30068-3
- Khoo CL, Chimoriya R, Simmons D, Piya MK. Partial meal replacement for people with type 2 diabetes: 2-year outcomes from an Australian general practice. Aust J Prim Health. 2022 Nov 2. doi: 10.1071/PY22180. Epub ahead of print. PMID: 36318919.
- Thakur A, Sharma D, Gupta B, Kramadhari N, Rajagopal R, Simmons D, Piya MK (2021) Severe obesity in a specialist type 2 diabetes outpatient clinic: an Australian retrospective cohort study. BMC Endocrine Disorders 21, 55. doi:10.1186/s12902-021-00722-9
