28th May 2023, Dr Chee L Khoo

Hypertriglyceridaemia has always played second fiddle to hypercholesterolaemia for a long time. Studies after studies have demonstrated the cardiovascular benefits of cholesterol lowering therapy. You might know that most of these clinical trials excluded patients with hypertriglyceridaemia. Does that mean that hypertriglyceridaemia doesn’t matter? We know hypertriglyceridaemia inflict oxidative damage to vital metabolic systems and organs. Unfortunately, clinical trials on triglyceride lowering therapy, in general, have conflicting results in demonstrating cardiovascular benefits. We now have a real-world study which demonstrated the role hypertriglyceridaemia play in end organ damage.
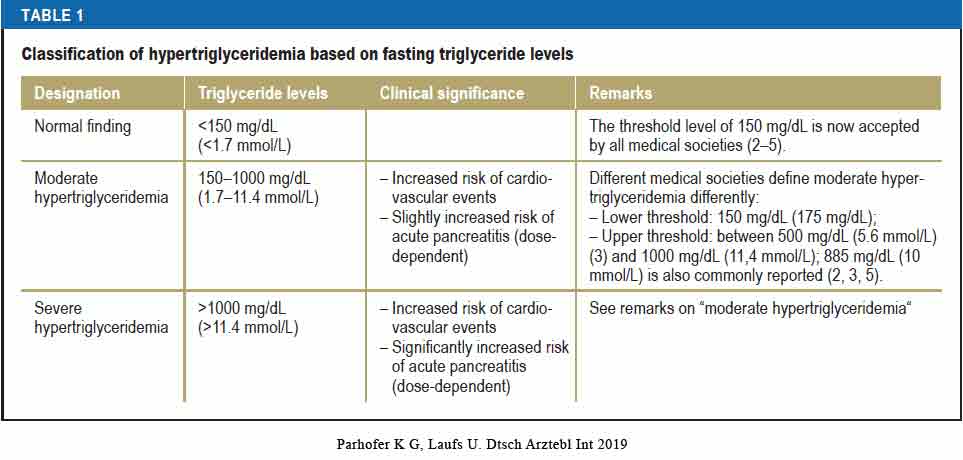
Hypertriglyceridaemia is closely associated with the presence of obesity, metabolic syndrome and diabetes mellitus. For instance, up to 50% of patients with type 2 diabetes have concomitant hypertriglyceridemia (1). Hypertriglyceridaemia varies in severity but there isn’t any formal classification of hypertriglyceridaemia but Table 1 is an attempt at classification of fasting TG levels. While we no longer have to worry about fasting cholesterol levels, it is still recommended that we check triglycerides in the fasting state.
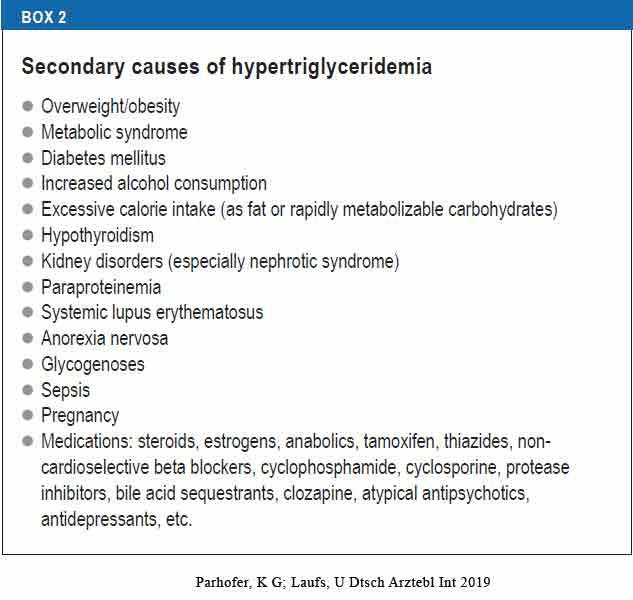
When we encounter hypertriglyceridaemia, we need to consider secondary causes. The common ones include diabetes (especially in patients with poor glycaemic control), excessive alcohol intake, hypothyroidism, high carbohydrate intake (especially, high glycaemic index carbohydrates) and certain drugs (especially anti-psychotics). A more comprehensive list is on Box 2.
How does hypertriglyceridaemia cause damage?
High levels of triglycerides have been shown to be independently correlated with high risk of atherosclerotic cardiovascular disease (ASCVD) [2] and all-cause mortality [3]. Trying to tease out whether the damage is from direct entry of triglycerides (TG) into the vascular tissues or from association with elevated cholesterol and lipoprotein is difficult. Don’t get me wrong. There is evidence that hypertriglyceridaemia has a causal role in cardiovascular disease.
In a large Mendelian meta-analysis comparing 20 000 patients with myocardial infarction to 500 000 control patients found that 1 standard deviation increase in triglyceride levels was associated with a 54% increase in the risk of myocardial infarction [4]. In another Mendelian randomisation analysis involving 654 783 participants, both lowering of triglycerides and LDL-C were associated with similar reduction of risk of coronary artery disease (5).
Thus, hypertriglycerides inflict damage whether on its own or in conjunction with cholesterol and the associated lipoproteins. Triglycerides are mainly hydrolysed by the lipoprotein lipase (LPL), and LPL and the cholesteryl ester transfer proteins hydrolyse its lipolytic products. These contain various molecules including large amounts of oxidised free fatty acids responsible for increasing the production of reactive oxygen species, decreasing nitric oxide, and increasing various adherence molecules and vascular cell adhesion molecules and other pro-inflammatory ones. This links them with other pro-inflammatory markers, such as interleukins TNF-cx, IL-1β. The excess TG is ingested by macrophages turning them into foam cells and further contribute to the inflammatory milieu. The inflammatory process associated with hypertriglyceridemia appeared to be the corner stone of hypertriglyceridemia-induced atherosclerosis.
There are further interactions of lipoprotein lipase with proteins such as apolipoprotein (apo), A-V, apo C-III, and angiopoietin-like proteins 3 and 4. These products on their own causes atherosclerotic damage. High TG also results in lower HDL-C levels, further adding to the lipid carnage.
The Japan EPA Lipid Intervention Study (JELIS) was an open label trial that compared a low dose (1.8 g per day) of eicosapentaenoic acid (EPA) with a low dose of statin (6). Although it showed a 19% reduction in cardiovascular events, the reduction is not related to reduction in LDL-C or TG levels.
The REDUCE-IT is a multicentre, randomised, double-blind, placebo-controlled trial comparing 2 g of icosapent ethyl twice daily with placebo in patients with established CVD or diabetes with other risk factors (7). It showed a 25% reduction in cardiovascular deaths or cardiovascular events. Once again, the reduction was not related to reduction in TG levels.
It is thought that the beneficial effects might be related to the effects of omega-3 fatty acid on plaque stabilisation and reduction in platelet activation and adhesion.
A most recent retrospective analysis investigated the role of hypertriglyceridaemia on renal function decline and development of end-stage kidney disease (ESKD) in a real-world clinical setting (8). A retrospective analysis of 3 Italian Local Health Unites was performed on patients with at least one plasma TG reading measured. The renal outcome was a reduction of >30% in eGFR from baseline and the development of end stage kidney disease (ESKD). Subjects were categorised as either normal (TG < 1.7 mmol/L), high (>5.65 mmol/L) or very high (TG >5.65 mmol/L).
There were 39,935, 5029 and 36 subjects with normal, high and very high TG respectively. The mean age of the subjects were 59.0 years, 44% were males and the prevalence of ASCVD were low. Subjects with very high TG tended to be younger and males. Those with high or very high TG expected had higher non-HDL cholesterol and lower HDL-C. Because our LDL-C is calculated from the Friedwald’s formula, LDL-C could not be calculated in subjects with very high TG.
Interestingly, patients with high TG were more likely to be on statins and hypertensive medications but not the subjects with very high TG. Both high TG groups were more likely to be on anti-diabetic medications suggesting a higher prevalence of diabetes with high TG.
During the 4.2 years of follow-up, the incidence rate/1000-person years of 27.1, 31.1 and 35.1 in the three groups respectively (P<0.01 for trend). There was also significantly higher incidence rate/1000-person years of ESKD in the high TG group as compared to the normal TG group was also recorded (0.9 vs 0.7; P<0.01).
When both renal outcomes (i.e. >30% GFR loss and ESKD) were combined (composite renal outcome) there was a linear trend toward greater incidence of worse outcome in the subgroups of subjects with progressively higher TG levels (27.4, 31.5 and 35.1 events per 1000 person-years in the group with normal, high and very high TG, respectively).
After univariate analysis, individuals with high TG had a 18% (p<0.001) and after multivariate analysis, individuals with high TG had a 49.8% (p<0.001) increased risk of eGFR reduction.
Those who went on to lose a greater amount of eGFR overtime had slightly higher HbA1c levels and comparable serum creatinine (but higher eGFR values) at baseline and were receiving a greater amount of cardiovascular therapeutic agents, namely statins, anticoagulants, antihypertensives and glucose lowering drugs. In other words, these were sicker subjects.
This study is not the first to associate high TG with decline in eGFR and ESKD. Tsuruya et al. in a large cohort of subjects from general population found that higher serum TG at baseline were significantly associated with a greater decline in eGFR during the 2-year study period, even after adjustment for confounding factors (9). Russo et al. [10]. reported an independent association between moderately elevated TGs and low HDL with de novo development of stage 3 CKD, i.e. either a sustained reduction of eGFR below 60 mL/min or new onset of albuminuria over a 4 year time period. in a 7 years retrospective study in older adults in China, Chen and coworkers reported that the HTG-waist phenotype (a clinical proxy of insulin resistance and the metabolic syndrome) was associated with an almost 30% excess risk of CKD even after adjustment for confounders [11].
In summary, hypertriglyceridaemia is associated with the risk of significant (>30%) decline in eGFR and ESKD. Furthermore, the higher the TG is, the higher the risk. Thus, when we encounter a patient with high TG, we need to take it seriously because not only does it contribute to decline in renal function, high TG inflict damage to the vascular systems and increase cardiovascular disease. We need to pay attention to the other CV risk factors as well. Improvement in glycaemic and blood pressure control will reduce the risk of cardiovascular mortality and morbidity.
References:
- Leiter LA, Lundman P, da Silva PM, et al.: Persistent lipid abnormalities in statin-treated patients with diabetes mellitus in Europe and Canada: results of the Dyslipidaemia International Study. Diabet Med 2011; 28: 1343–51
- Sarwar N, Danesh J, Eiriksdottir G, et al. Triglycerides and the risk of coronary heart disease: 10,158 incident cases among 262,525 participants in 29 Western prospective studies. Circulation 2007; 115:450-458.
- Nordestgaard BG, Benn M, Schnohr P, et al. Nonfasting triglycerides and risk of myocardial infarction, ischemic heart disease, and death in men and women. JAMA 2007; 298:299-308.
- Musunuru K, Kathiresan S. Surprises from genetic analyses of lipid risk factors for atherosclerosis. Circ Res 2016; 118:579-585
- Ference BA, Kastelein JJ, Ray KK, et al. Association of triglyceride-lowering LPL variants and LDL-C-lowering LDLR variants with risk of coronary heart disease. JAMA 2019; 321 :364-373.
- Yokoyama M, Origasa H, Matsuzaki M, et al. Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomised open-label, blinded endpoint analysis. Lancet 2007; 369: 1090-1098.
- Deepak L Bhatt, MD, MPH, FESC, REDUCE-IT: Residual Cardiovascular Risk in Statin-Treated Patients with Elevated Triglycerides: Now We Can REDUCE-IT!, European Heart Journal, Volume 40, Issue 15, 14 April 2019, Pages 1174–1175, https://doi.org/10.1093/eurheartj/ehz179
- Pontremoli R, Desideri G, Arca M, Temporelli PL, Perrone V, Dovizio M, Borghi C, Esposti LD; on the behalf of Local Health Units Group. Hypertriglyceridemia is associated with decline of estimated glomerular filtration rate and risk of end-stage kidney disease in a real-word Italian cohort: Evidence from the TG-RENAL Study. Eur J Intern Med. 2023 May;111:90-96. doi: 10.1016/j.ejim.2023.02.019. Epub 2023 Mar 10. PMID: 36906475.
- Tsuruya K, Yoshida H, Nagata M, et al. Association of the triglycerides to high density lipoprotein cholesterol ratio with the risk of chronic kidney disease: analysis in a large Japanese population. Atherosclerosis 2014;233(1):260–7. https://doi.org/10.1016/j.atherosclerosis.2013.12.037
- Russo GT, De Cosmo S, Viazzi F, et al. Plasma triglycerides and HDL-C levels predict the development of diabetic kidney disease in subjects with type 2 diabetes: the AMD annals initiative. Diabet Care 2016;39(12):2278–87. https://doi.org/10.2337/dc16-1246.
- Chen R, Sun G, Liu R, et al. Hypertriglyceridemic waist phenotype and risk of chronic kidney disease in community-dwelling adults aged 60 years and older in Tianjin, China: a 7-year cohort study. BMC Nephrol 2021;22(1):182. https://doi.org/10.1186/s12882-021-02339-5
