12th July 2024, A/Prof Chee L Khoo
We are always on the look out for the traditional cardiovascular risk factors – hypertension, diabetes, lipids and smoking to reduce the risk of adverse cardiovascular events. These are termed standard modifiable cardiovascular risk factors (SMuRFs). Unfortunately, there are a significant number of patients that present with acute coronary syndrome (ACS) who has none of the SMuRFs. Or at least risk factors not reaching the current accepted thresholds for diagnosis and the initiation of primary prevention therapy. In fact, these SMuRF-less ACS make up 17% of all ACS in a meta-analysis of 14 clinical trials (1). Who are these patients? Unfortunately, they have a higher early mortality rate (2). We have to understand these SMuRF-less patients better to help reduce that mortality rate.
So, what are the SMuRFs? These are risk factors in primary prevention setting – BP ≤140/90 mmHg, diabetes, current smoker or smoking within last 12 months, total cholesterol > 5.5 mmol/L and LDL-C > 3.5 mol/L. Of course, those target numbers will drop after the first ACS. Up until recently, this group has not attracted much attention in our secondary prevention efforts.
In the Australian GRACE (Global Registry of Acute Coronary Events) and CONCORDANCE (Cooperative National Registry of Acute Coronary Events) Registry cohorts of 3,081 participants, STEMI patients without SMuRFs were observed to have a higher in-hospital mortality compared to their counterparts with SMuRFs (6% vs 4%) (3).
This finding was similar to the larger Swedish national cardiac registry, SWEDEHEART (Swedish Web-system for Enhancement and Development of Evidence-based care in Heart disease Evaluated According to Recommended Therapies) (4). In this cohort of >60,000, ST Elevation Myocardial Infarction (STEMI) patients, women without SMuRFs had a high 30-day mortality (19%) compared to women ≥1 SMuRFs (11%) (p < 0.0001). A higher mortality risk was also seen in male patients without SMuRFs (10% vs 6%) (p < 0.0001).
The higher early mortality was thought to be at least partially attributable to a lower rate of prescription of angiotensin-converting enzyme inhibitors (ACEi), angiotensin receptor blocker (ARB), and beta-blockers in STEMI patients without SMuRFs, and it appeared to be driven by sudden arrhythmic death.
Guidelines have been preoccupied with getting those SMuRF to target but the data about and understanding of these SMuRF-less is quite limited. Thus, evidence for optimal management of patients who are SMuRF-less is lacking. An expert panel composed of 17 internationally recognised cardiovascular disease leaders were convened late last year to develop a consensus clinical pathway that outlines additional investigations and management to improve the care of these patients (5).
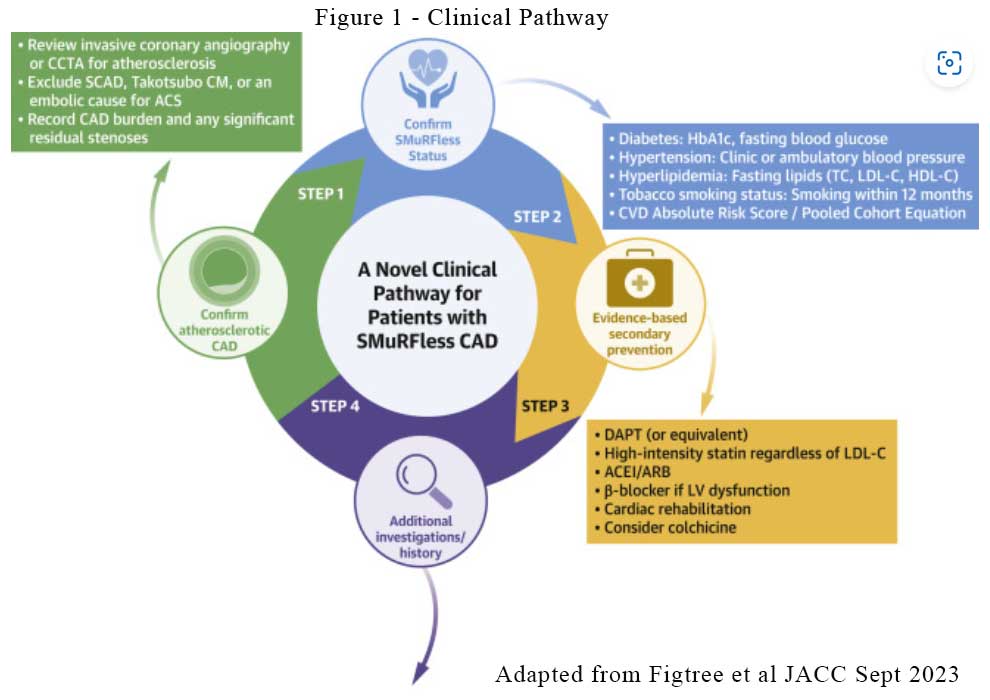
There are 4 steps in the clinical pathway:
- Confirm coronary event
- Confirm SMuRF-less status (Ambulatory BP monitoring is recommended)
- Institute usual evidence-based secondary prevention management including much lower LDL-C (< 1.8mmol/L or 1.4mmol/L in high risk patients), ACEi/ARB, beta-blockers and possibly colchicine.
- Start investigating for “rarer” causes of CAD (see Figure 1)
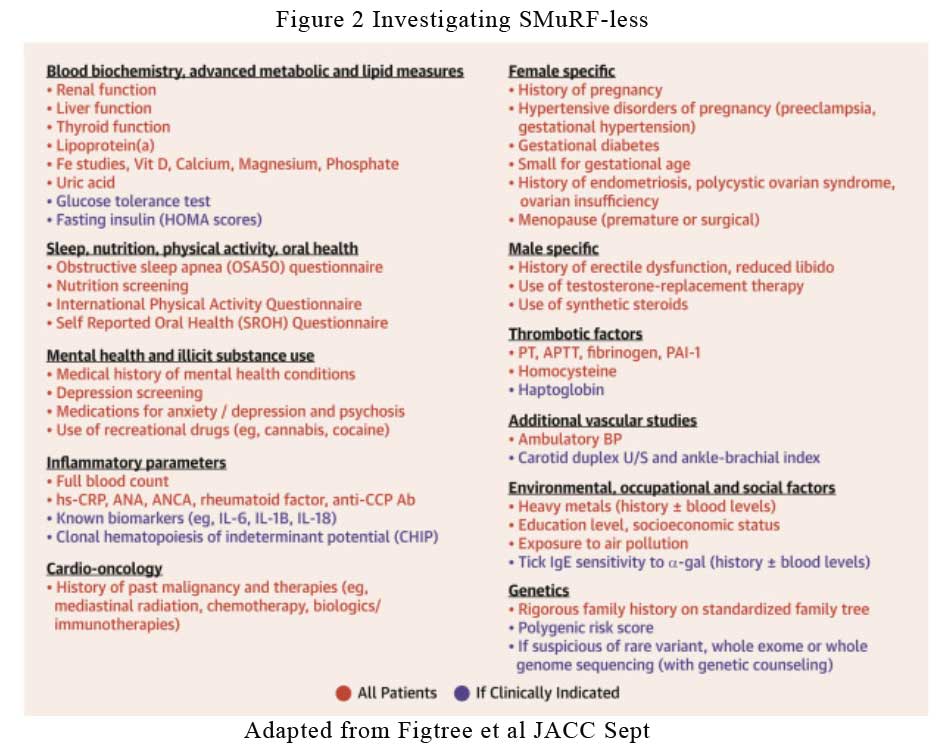
In addition to the usual secondary prevention management, we need to consider and act on:
- Obesity
- Obstructive sleep apnoea
- Nutrition (especially saturated fats)
- Physical activity
- Oral/periodontal health
- Psychosocial factors
- Inflammatory conditions including the various arthropathy and their immunotherapy agents
- Thrombotic factors including platelet dysfunction, hyperhomocysteinemia
- Other vascular conditions including CKD, PAD
- Lipoprotein (a)
- Environmental factors including heavy metal exposure, air pollution
See Figure 2.
The proportion of SMuRF-less ACS has been rising steadily over the last 20 years, from 11% in 2006 to 27% in 2014 (3). One of the reasons for the increase is that perhaps, we have identified many our patients with those SMuRF and treated those risk factors, thus preventing the adverse cardiovascular events. What is left behind are those that are SMuRF-less. Nonetheless, there are at 1:4 of our patients with ACS that we could not have prevented because they are not the usual suspects. It may also mean that our targets of those traditional risk factors might be too high. This might be especially true for lipid targets. Or perhaps, these patients have other less common risk factors or causes that we have yet to look into.
In primary care, there are also opportunities for primary prevention in patients with the above non-SMuRF factors especially lipoprotein (a). The presence of many of these risks mandate a lower LDL-C target than the 3.5mmol/L even before the first ACS. While waiting for the evidence to emerge, it is important to adhere to the secondary prevention guidelines. Australia is leading the way with a number of SMuRF-less CAD clinics already established to provide 5-year clinical outcomes data and facilitate analyses of the cost-effectiveness of diagnosis and treatment. Primary prevention is what we do best in primary care. We will need to conduct more prior investigations to prevent the first event.
References:
- Khot U.N., Khot M.B., Bajzer C.T., Sapp S.K., Ohman E.M., Nrener S.J. et al. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA. 2003; 290: 898-904
- Figtree GA, Vernon ST, Hadziosmanovic N, Sundström J, Alfredsson J, Arnott C et al. Mortality in STEMI patients without standard modifiable risk factors: a sex-disaggregated analysis of SWEDEHEART registry data. Lancet. 2021; 397: 1085-1094
- S.T. Vernon, S. Coffey, M. D’Souza, et al. ST-segment-elevation myocardial infarction (STEMI) patients without standard modifiable cardiovascular risk factors—how common are they, and what are their outcomes? J Am Heart Assoc, 8 (2019), Article e013296
- G.A. Figtree, S.T. Vernon, N. Hadziosmanovic, et al. Mortality in STEMI patients without standard modifiable risk factors: a sex disaggregated analysis from the SWEDEHEART registry Lancet, 397 (10279) (2021), pp. 1085-1094
- Figtree GA, Vernon ST, Harmer JA, Gray MP, et al. Clinical Pathway for Coronary Atherosclerosis in Patients Without Conventional Modifiable Risk Factors: JACC State-of-the-Art Review. J Am Coll Cardiol. 2023 Sep 26;82(13):1343-1359.
