23rd December 2024, A/Prof Chee L Khoo
The reference values for serum magnesium (Mg2+) have been proposed to be somewhere between ~0.6 and ~1.2 mmol/L in healthy humans. That is a pretty wide range. Have you noticed that every second person discharged from hospital is recommended to take some Mg2+ supplement. Serum Mg2+ is often (or always) checked in hospitalised patients. Yet, there is no recommendations in guidelines that we routinely check serum Mg2+ in all patients. Should we? Are we missing something important?
The Canadian Health Measure Survey Cycle 3, conducted in 2012–2013, measured serum magnesium in subjects aged 3–79 years. 9.5% – 16.6% of adults and 15.8% – 21.8% of adolescents had serum magnesium concentrations < 0.75 mmol/L [1], which is a level currently accepted as an indication of magnesium deficiency. However, it has recently been suggested that maybe this indicative value is likely to be too low and should be raised to <0.85, as values in this range are associated with increased health risks. Let’s see why later.
What is Mg2+ for?
Mg2+ + has many physiological functions including
- Maintaining DNA and RNA stability
- Regulating cellular proliferation
- Bone metabolism
- Neuromuscular functioning [2,3]
- Regulating inflammation [4], and
- Maintaining haemostasis
See Figure 1.
Magnesium homeostasis
Mg2+ is primarily absorbed through the intestinal tract. The major food sources include those of plant origin such as grains, vegetables, and pulses. Partly fermentable fibres or non-fermentable fibres inhibit while low- or indigestible carbohydrates increases absorption. High fibre intakes (40-50 g/day) lower magnesium absorption, probably because of the magnesium-binding action of the phytate phosphorus associated with the fibre (5-7). High intakes of zinc at 142 mg/day reduce absorption (8). When protein intake is less than 30 g/day (9), magnesium absorption decreases. When protein intake is greater than 94 g/day, renal magnesium excretion may increase (10), although adaptation may occur. Industrial food processing reduces the availability and absorption of Mg2+.
60% of Mg2+ is stored in bones, mostly within and on the surface of hydroxyapatite crystals. The portion in the crystals is released only following bone resorption. Mg2+ deficiency affects the structure of bone, causing large hydroxyapatite crystals. It affects the cells involved in bone turnover, osteoblasts, and osteoclasts. Dietary magnesium intake has been linked to bone mineral density and serum magnesium levels are strongly associated with an increased risk of fractures and osteoporosis [11-12].
Overall Mg2+ maintenance and homeostasis are most likely regulated through excretion. Some of the filtered Mg2+ is reabsorbed passively in the proximal tubule but most is reabsorbed actively in the ascending loop of Henle related to the reabsorption of NaCl.
As most of the Mg2+ is in storage in the bones, serum Mg2+ is a poor indicator of Mg2+ status. In the magnesium retention test, Mg2+ excretion is measured following an infused Mg2+ load. Alternatively, urinary Mg2+ or magnesium/creatinine ratio in spot urine or in 24 h urine collection can be performed.
Mg2+ deficiency and diseases
Mg2+deficiency has been shown to be associated with a diverse number of cardiovascular and metabolic conditions including diabetes, prediabetes, obesity, cardiovascular diseases and bone health. It would be naïve to assume that Mg2+ supplementation should be beneficial but conclusive data is rather patchy. Let’s see what we have in evidence.
Metabolic conditions
Patients with diabetes (whether T1D or T2D) are more likely to have a low serum magnesium (<0.66 mmol/L) than control those without diabetes. Poor glycaemic control can lead to low Mg2+. HbA1c levels have been shown to negatively correlate with serum magnesium concentration in people with T1DM [13,14] but recent studies did not find that correlation (15). Oost et al. noted that hypomagnesaemia seemed to be linked to glycaemia control only in patients who required high levels of insulin and have evidence of insulin resistance [16].
Which is the chicken and which is the egg? In a cohort study, hypomagnesaemia (<0.7 mmol/L) is more common in patients with T2DM but not pre-diabetes (17). Yet, Fang et al found that increasing dietary magnesium intake is associated with a reduced risk of stroke, heart failure, diabetes (18). A number of meta-analyses have reported associations between hypomagnesaemia and the development of T2D (19,20).
Once, diabetes has developed, magnesium deficiency has been shown to worsen the complications of the disease, whilst conversely, magnesium supplementation has been shown to protect against complications [21].
Cardiovascular health
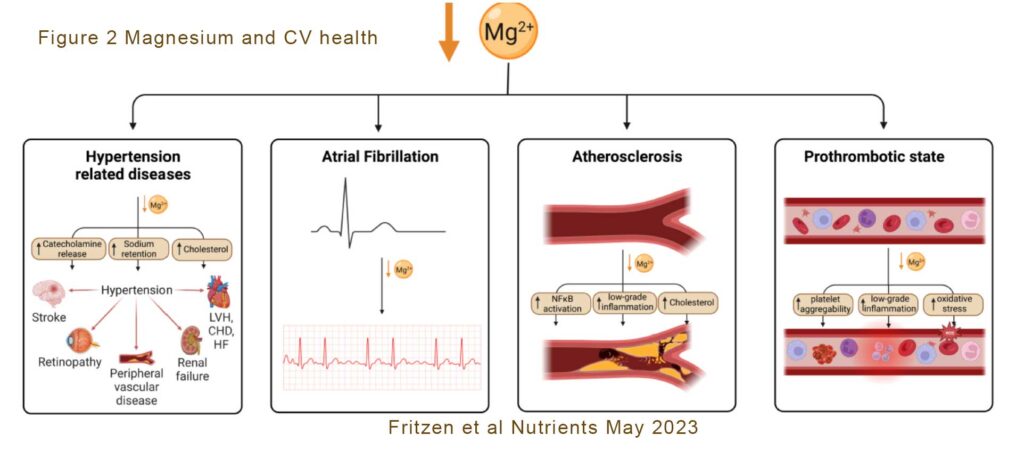
Magnesium is an essential nutrient for cardiovascular health, acting to regulate vascular smooth muscle, cardiac conduction, vascular endothelial cell functioning, and thrombosis (coagulation and platelet aggregation pathways). Hypomagnesaemia and low dietary magnesium intake increase the likelihood of developing coronary artery disease (CAD) [22]. Hypomagnesaemia has been associated with hypertension, which can lead to congestive heart failure (CHF) or CAD. See Figure 2.
There have been numerous studies reporting inverse relationships between dietary Mg2+ and blood pressure and/or hypertension. In the international randomised controlled clinical trial, MagPie, pregnant women given magnesium sulphate had a 58% lower risk of pre-eclampsia than placebo (23).
Some studies have shown a causal relationship between high magnesium levels and lower risk of CAD which others have not (24,25). The association between hypomagnesaemia and increased risk of AF is more robust. A long-term longitudinal study which followed 3550 people for over 20 years with no prior history of cardiovascular disease found a moderate association between hypomagnesaemia and AF diagnosis (26). Similar association have been found with QT prolongation and other conduction abnormalities (27).
Because of the role of magnesium in myocardial contraction, you would expect an association between hypomagnesaemia and heart failure. Yet the number of studies exploring that is limited. In the 4th International Study of Infarct Survival (ISIS-4) 58,050 patients who had a acute myocardial infarction were randomised to either captopril, mononitrate, iv magnesium or placebo (28). Magnesium did not improve mortality. In the 2nd Leicester Intravenous Magnesium Intervention trial (LIMIT-2), 2316 patients who had just had an acute AMI were randomised to receive either iv magnesium or placebo prior to their thrombolytic therapy. Magnesium reduced mortality from IHD by 21% (29, 30).
Who needs Mg2+ checked?
In the meantime, perhaps, we need to check serum magnesium more frequently especially in patients with metabolic disorders (e.g diabetes or prediabetes), cardiovascular diseases (including CAD, HF, conduction defects) and thromboembolic disorders (including AF).
How much do we need?
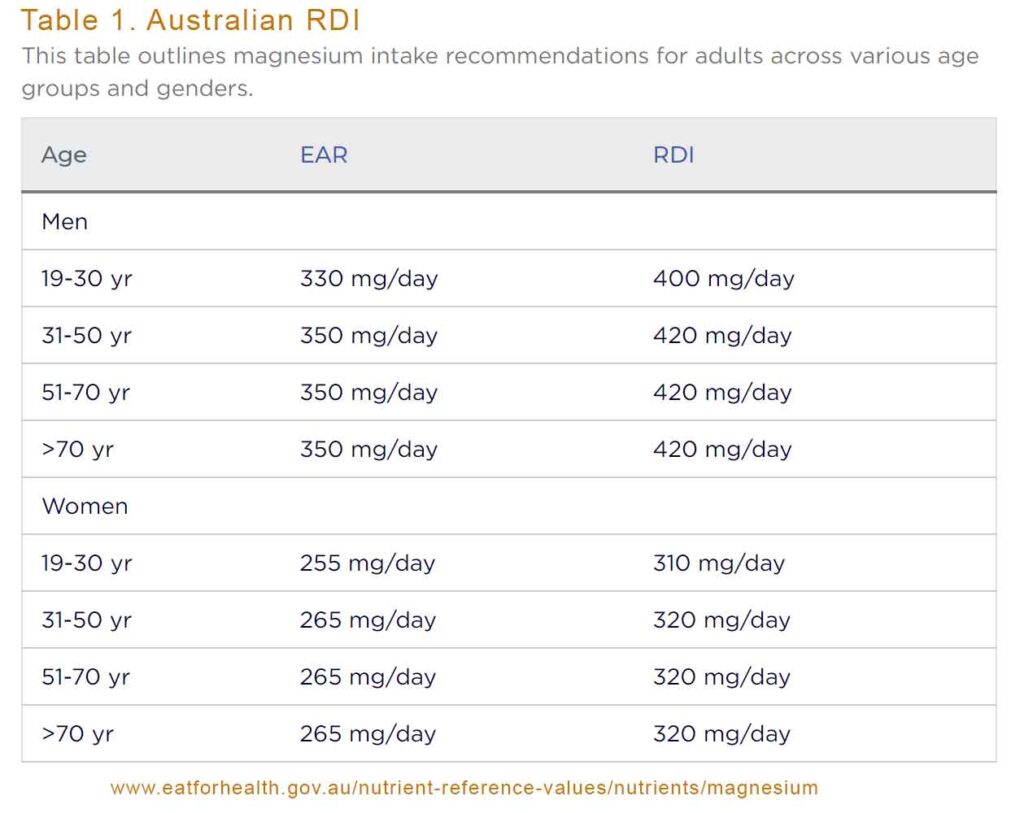
As we said at the outset of this article, the data on the harms of hypomagnesaemia is beginning to take shape and data on the benefits of magnesium supplementation is increasing. What is normal is not always easy to ascertain. According to Australian RDI recommendations, adult men needs a little over 400mg per day while women needs a little over 300mg per day (31). See Table 1. Pregnant and lactating women needs a tad under 400mg per day.
The normal reference range for the magnesium in blood serum is 0.76–1.15 mmol/L although some recommend that patients with diabetes needs to aim for levels higher than 0.85 mmol/L. Lower magnesium levels appear to be associated with a more rapid decline of renal function in patients with type 2 diabetes. Patients with serum magnesium levels between 0.82 and 1.03 mmol/L had the lowest deterioration of renal function and the best glycemic control [32,33].
Thus, there is increasing evidence linking the hypomagnesaemia with metabolic, vascular and thrombotic diseases. Many of the studies were smaller studies with short duration. The choice of magnesium salts was also different in different studies. Well-designed and adequately powered studies are therefore urgently needed to fully understand the impact of magnesium deficiency and the potential benefits of magnesium supplementation on vascular pathology, cardiac function and the haemostatic process, particularly in higher-risk groups such as individuals with diabetes.
References:
- Bertinato, J.; Wang, K.C.; Hayward, S. Serum magnesium concentrations in the Canadian population and associations with diabetes, glycemic regulation, and insulin resistance. Nutrients 2017, 9, 296.
- Maier, J.A.M.; Locatelli, L.; Fedele, G.; Cazzaniga, A.; Mazur, A. Magnesium and the brain: A focus on neuroinflammation and neurodegeneration. Int. J. Mol. Sci. 2022, 24, 223.
- Kirkland, A.E.; Sarlo, G.L.; Holton, K.F. The role of magnesium in neurological disorders. Nutrients 2018, 10, 730.
- Maier, J.A.; Castiglioni, S.; Locatelli, L.; Zocchi, M.; Mazur, A. Magnesium and inflammation: Advances and perspectives. Semin. Cell Dev. Biol. 2021, 115, 37–44.
- Kelsay JL, Bahall KM, Prather ES. Effect of fiber from fruit and vegetables on the metabolic responses of human subjects. Am J Clin Nutr 1979;32:1876-80
- McCance RA, Widdowson EM. Mineral metabolism on dephytinised bread. J Physiol 1942a;101:304-13.
- McCance RA, Widdowson EM. Mineral metabolism in healthy adults on white and brown bread dietaries. J Physiol 1942b;101:44-85
- Spencer H, Norris C, Williams D. Inhibitory effect of zinc on magnesium balance and absorption in man. J Am Coll Nutr 1994b;13:479-84
- Hunt SM, Schofield FA. Magnesium balance and protein intake in adult human female. Am J Clin Nutr 1969;22:367-73
- Mahalko JR, Sandstead HH, Johnson LK, Milne DB. Effect of a moderate increase in dietary protein on the retention and excretion of Ca, Cu, Fe, Mg, P and Zn by adult males. Am J Clin Nutr 1983;37:8-14.
- Ismail, A.A.A.; Ismail, Y.; Ismail, A.A. Chronic magnesium deficiency and human disease; time for reappraisal? QJM 2018, 111, 759–763.
- 34. Castiglioni, S.; Cazzaniga, A.; Albisetti, W.; Maier, J.A. Magnesium and osteoporosis: Current state of knowledge and future research directions. Nutrients 2013, 5, 3022–3033.
- Rodrigues, A.K.; Melo, A.E.; Domingueti, C.P. Association between reduced serum levels of magnesium and the presence of poor glycemic control and complications in type 1 diabetes mellitus: A systematic review and meta-analysis. Diabetes Metab. Syndr. 2020, 14, 127–134.
- 72. Sobczak, A.I.S.; Stefanowicz, F.; Pitt, S.J.; Ajjan, R.A.; Stewart, A.J. Total plasma magnesium, zinc, copper and selenium concentrations in type-I and type-II diabetes. Biometals 2019, 32, 123–138.
- van Dijk, P.R.; Waanders, F.; Qiu, J.; de Boer, H.H.R.; van Goor, H.; Bilo, H.J.G. Hypomagnesemia in persons with type 1 diabetes: Associations with clinical parameters and oxidative stress. Ther. Adv. Endocrinol. Metab. 2020, 11, 2042018820980240.
- 74. Oost, L.J.; van Heck, J.I.P.; Tack, C.J.; de Baaij, J.H.F. The association between hypomagnesemia and poor glycaemic control in type 1 diabetes is limited to insulin resistant individuals. Sci. Rep. 2022, 12, 6433.
- Simmons, D.; Joshi, S.; Shaw, J. Hypomagnesaemia is associated with diabetes: Not pre-diabetes, obesity or the metabolic syndrome. Diabetes Res. Clin. Pract. 2010, 87, 261–266.
- Fang, X.; Wang, K.; Han, D.; He, X.; Wei, J.; Zhao, L.; Imam, M.U.; Ping, Z.; Li, Y.; Xu, Y.; et al. Dietary magnesium intake and the risk of cardiovascular disease, type 2 diabetes, and all-cause mortality: A dose-response meta-analysis of prospective cohort studies. BMC Med. 2016, 14, 210.
- Kim, D.J.; Xun, P.; Liu, K.; Loria, C.; Yokota, K.; Jacobs, D.R., Jr.; He, K. Magnesium intake in relation to systemic inflammation, insulin resistance, and the incidence of diabetes. Diabetes Care 2010, 33, 2604–2610.
- Villegas, R.; Gao, Y.T.; Dai, Q.; Yang, G.; Cai, H.; Li, H.; Zheng, W.; Shu, X.O. Dietary calcium and magnesium intakes and the risk of type 2 diabetes: The Shanghai Women’s Health Study. Am. J. Clin. Nutr. 2009, 89, 1059–1067
- Feng, J.; Wang, H.; Jing, Z.; Wang, Y.; Cheng, Y.; Wang,W.; Sun, W. Role of magnesium in type 2 diabetes mellitus. Biol. Trace Elem. Res. 2020, 196, 74–85.
- Tangvoraphonkchai, K.; Davenport, A. Magnesium and cardiovascular disease. Adv. Chronic Kidney Dis. 2018, 25, 251–260.
- The Magpie Trial Collaboration Group. Do women with pre-eclampsia, and their babies, benefit from magnesium sulphate? The Magpie Trial: A randomised placebo-controlled trial. Lancet 2002, 359, 1877–1890.
- Larsson, S.C.; Burgess, S.; Michaëlsson, K. Serum magnesium levels and risk of coronary artery disease: Mendelian randomisation study. BMC Med. 2018, 16, 68.
- He, B.; Xia, L.; Zhao, J.; Yin, L.; Zhang, M.; Quan, Z.; Ou, Y.; Huang, W. Causal Effect of Serum Magnesium on Osteoporosis and Cardiometabolic Diseases. Front. Nutr. 2021, 8, 738000.
- Khan, A.M.; Lubitz, S.A.; Sullivan, L.M.; Sun, J.X.; Levy, D.; Vasan, R.S.; Magnani, J.W.; Ellinor, P.T.; Benjamin, E.J.; Wang, T.J. Low serum magnesium and the development of atrial fibrillation in the community: The Framingham heart study. Circulation 2013, 127, 33–38. [CrossRef]
- Topol, E.J.; Lerman, B.B. Hypomagnesemic torsades de pointes. Am. J. Cardiol. 1983, 52, 1367–1368.
- ISIS-4: A randomised factorial trial assessing early oral captopril, oral mononitrate, and intravenous magnesium sulphate in 58,050 patients with suspected acute myocardial infarction. ISIS-4 (Fourth International Study of Infarct Survival) Collaborative Group. Lancet 1995, 345, 669–685.
- Woods, K.L.; Fletcher, S.; Roffe, C.; Haider, Y. Intravenous magnesium sulphate in suspected acute myocardial infarction: Results of the second Leicester Intravenous Magnesium Intervention Trial (LIMIT-2). Lancet 1992, 339, 1553–1558.
- 150. Woods, K.L.; Fletcher, S. Long-term outcome after intravenous magnesium sulphate in suspected acute myocardial infarction:The second Leicester Intravenous Magnesium Intervention Trial (LIMIT-2). Lancet 1994, 343, 816–819.
- https://www.eatforhealth.gov.au/nutrient-reference-values/nutrients/magnesium. Accessed 23/12/2024.
- Pham P.C., Pham P.M., Pham P.A., Pham S.V., Pham H.V., Miller J.M., Yanagawa N., Pham P.T. Lower serum magnesium levels are associated with more rapid decline of renal function in patients with diabetes mellitus type 2. Clin. Nephrol. 2005;63:429–436.
- 58.Pham P.C., Pham P.M., Pham S.V., Miller J.M., Pham P.T. Hypomagnesemia in patients with type 2 diabetes. Clin. J. Am. Soc. Nephrol. 2007;2:366–373.
