12th June 2025, NIA Diagnostic Imaging
Papillary thyroid carcinoma (PTC) is the most prevalent type of thyroid malignancy, accounting for approximately 75–90% of all thyroid cancer cases (Cozens, 2011; Solbiati et al., 2017). These tumours are typically slow-growing and display distinctive histologic features, including papillary structures, nuclear alterations, and multiple subtypes (Gonzalez-Gonzalez et al., 2011; Limaiem et al., 2023). The prognosis is generally favourable, with survival rates exceeding 90% and low mortality rates, ranging from 4–8% (Cozens, 2011; Solbiati et al., 2017).
PTC is most commonly diagnosed between the third and seventh decades of life, with an average age of diagnosis around 50 years (Solbiati et al., 2017; Limaiem et al., 2023). It occurs more frequently in women, with a female-to-male ratio of approximately 3:1 (Limaiem et al., 2023). A history of ionising radiation exposure is the most significant risk factor (Brito et al., 2016), while other contributing factors include a personal or family history of thyroid disease, obesity, and excessive dietary iodine intake (Limaiem et al., 2023; Ross et al., 2023).
Prognostic outcomes are influenced by several clinical and pathological variables including;
- Patient age
- Tumour size
- Histological subtype
- Lymph node involvement
- Extrathyroidal extension
- Distant metastasis
(Gonzalez-Gonzalez et al., 2011).
SYMPTOMS/PATIENT PRESENTATION
Clinically, PTC often presents as a painless, firm neck nodule, which may be discovered during self-examination, physical evaluation, or incidentally on imaging (Ross et al., 2023). Symptoms such as difficulty swallowing, breathing difficulties, voice changes, or cervical lymphadenopathy may also occur. A hard, fixed thyroid mass with regional lymphadenopathy is strongly suggestive of malignancy (Bailey & Wallwork, 2018).
Epidemiological studies have found that prior benign thyroid conditions—such as thyroiditis, goitre, and nodules—are associated with an increased risk of developing thyroid cancer (Kitahara et al., 2018). While most PTC cases are sporadic, a positive family history accounts for approximately 5–15% of cases (Bailey & Wallwork, 2018; Byun et al., 2020).
THE ROLE OF ULTRASOUND
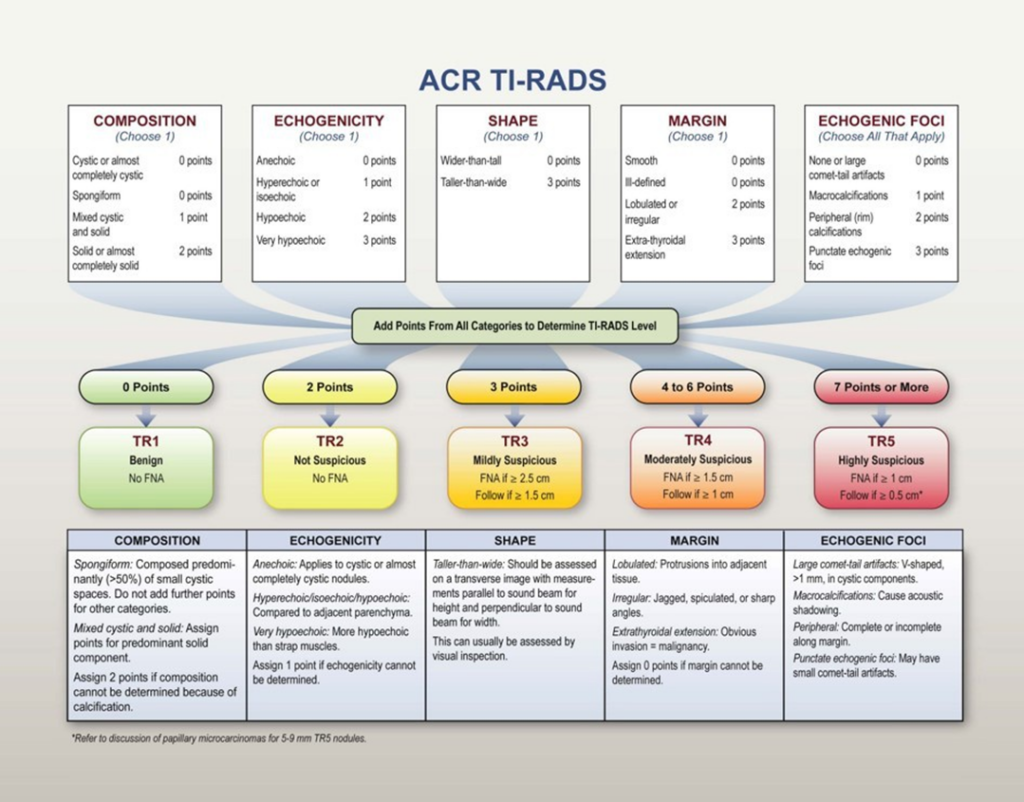
Ultrasound plays a central role in the detection, risk stratification, and monitoring of thyroid nodules and suspected thyroid malignancies. The American College of Radiology’s Thyroid Imaging Reporting and Data System (ACR TI-RADS) provides a structured and standardised approach for assessing thyroid nodules based on sonographic features. It offers guidance on follow-up imaging and the need for fine- needle aspiration biopsy (American College of Radiology, n.d.).
Ultrasound enables the assessment of key characteristics such as echogenicity, composition, shape, margin definition, and the presence of calcifications—all of which contribute to malignancy risk scoring. Additionally, ultrasound is essential for evaluating cervical lymph nodes and detecting suspicious features such as cystic changes or microcalcifications (Rhys, 2011).
Reviewing previous imaging is crucial to ensure consistency in follow-up and detect interval changes over time (Tamhane & Gharib, 2016). While thyroid-stimulating hormone (TSH) levels are not specific for cancer detection, they help identify underlying benign thyroid disorders such as hypothyroidism or hyperthyroidism (Bailey & Wallwork, 2018). Reviewing prior biopsy results is also critical in guiding management decisions and reducing unnecessary repeat procedures (Bailey & Wallwork, 2018).
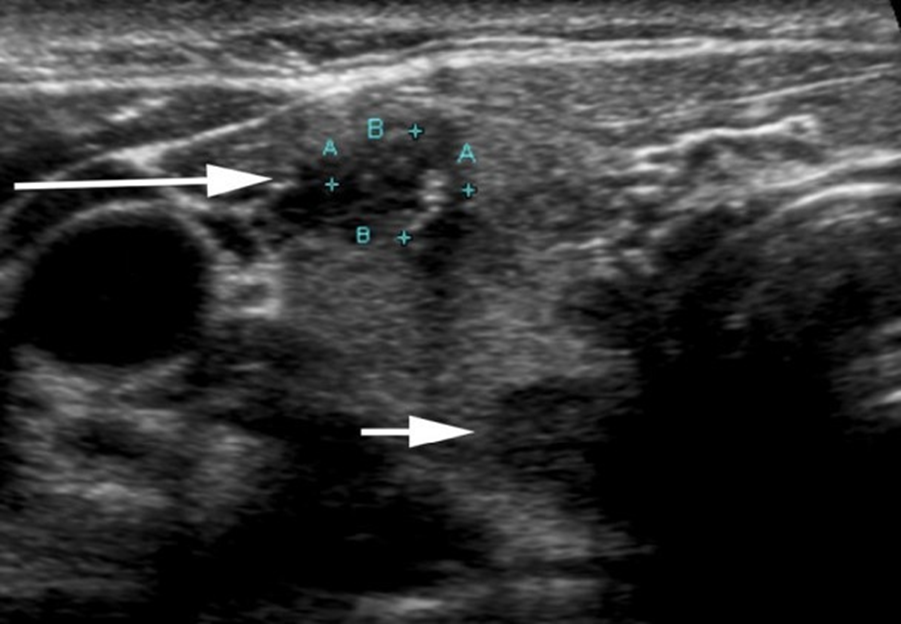
Figure 1 demonstrates a transverse image of the upper pole of the right thyroid lobe of 52-year-old female with a history of multi-nodular goiter (Ghai et al., 2021). In this image, the long white arrow indicates a 6 mm hypoechoic irregular bordered PTC nodule with microcalcifications, and the short white arrow indicates a hypoechoic well-defined benign nodule. (Ghai et al., 2021).
CONCLUSION
In summary, PTC is a common and treatable thyroid malignancy with a favourable prognosis. Ultrasound is an indispensable imaging modality for its initial evaluation and long-term management. Ultrasound is a safe, cost-effective, and highly sensitive tool for diagnosis, risk assessment, and surveillance of thyroid carcinoma. At NIA Diagnostic Imaging our friendly team are always happy to arrange same- day appointments for thyroid imaging. Proudly, NIA Diagnostic Imaging will also bulk-bill thyroid biopsies for our patients.
References:
American College of Radiology. ( n. d.). ACR TI-RAD. https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/TI-RADS Australasian Sonographers Association. (2022). ASA Sonographer Code of Conduct. https://www.sonographers.org/publicassets/0c00c285-1c6f-ea11-90fb-0050568796d8/ASA_Code_of_Conduct_2015.pdf
Bailey, S., & Wallwork, B. (2018). Differentiating between benign and malignant thyroid nodes: an evidence-based approach in general practice. Australian Journal of General Practice, 47(11). doi:10.31128/AJGP-03-18-4518
Brito, J. P., Hay, I. D., & Foote, R. L. (2016). Thyroid cancer. In L. L., Gunderson, & J. E., Tepper (Eds.), Clinical Radiation Oncology (4th ed., pp. 715-730). Elsevier.
Byun, S. -H., Min, C., Choi, H. -G., & Hong, S. -J. (2020). Association between family histories of thyroid cancer and thyroid cancer: A cross-sectional study using the Korean genome and epidemiology study data. Genes, 11(9). doi:10.3390/genes11091039
Cozens, N. (2011). Thyroid and parathyroid. In P. L. Allan, G. M. Baxter, & M. J. Weston (Eds.). Clinical ultrasound (3rd ed., pp. 867- 889). Elsevier.
Ghai, S., O’Brien, C., Goldstein, D. P., & Sawka, A. M. (2021). Ultrasound in active surveillance for low-risk papillary thyroid cancer: imaging considerations in case selection and disease surveillance. Insights into imaging, 12(130). 10.1186/s13244-021-01072-9 Gonzalez-Gonzalez, R., Bologna-Molina, R., Carreon-Burciaga, R. G., Gómezpalacio-Gastelum, M., Molina-Frechero, & Salazar- Rodríguez, S. (2011). Papillary thyroid carcinoma: A differential diagnosis and prognostic values of its different variants: Review of the literature. International Scholarly Research Notices, 2011. doi:10.5402/2011/915925
Kitahara, C. M., Farkas, D. K., Jørgensen, J. O. L., Cronin-Fenton, D., & Sørensen, H. T. (2018). Benign thyroid diseases and risk of thyroid cancer: A nationwide cohort study. The Journal of Clinical Endocrinology and metabolism, 103(6), 2216-2224. doi:10.1210/jc.2017-02599
Limaiem, F., Rehman, A., Anastasopoulou, C., & Mazzoni, T. (2023). Papillary thyroid carcinoma. StatPearls. StatPearls Publishing. Retrieved Aug 10, 2023, from https://www.ncbi.nlm.nih.gov/books/NBK536943/
Ross, J., Parmar H. A., Avram, A., Ibrahim, M., & Mukherji, S. K. (2023). Imaging in thyroid cancer. In P. M., Silverman (Ed.). Oncologic imaging: a multidisciplinary approach (2nd ed., pp. 616-629). Elsevier.
Rhys, R. (2011). Cervical lymph nodes. In P. L. Allan, G. M. Baxter, & M. J. Weston (Eds.). Clinical ultrasound (3rd ed., pp. 920-937). Elsevier.
Solbiati, L., Charboneau, J. W., Cantisani, V., Reading, C., Mauri, G. (2017). The thyroid gland. In C. M. Rumack & D. Levine (Eds.), Diagnostic ultrasound (5th ed., pp. 691-731). Elsevier.
Tamhane, S., & Gharib, H. (2016). Thyroid nodule update on diagnosis and management. Clinical Diabetes and Endocrinology, 2(17). doi: 10.1186/s40842-016-0035-7