14th October 2025, NIA Diagnostic Imaging
Breast cancer is a major public health issue. It is the most common cancer in Australian women and the second most common cancer overall (Breast Cancer Network Australia, n.d.). Breast markers (or clips) are small (2–3 mm) biocompatible metallic or bioabsorbable markers placed in a breast lesion or area of abnormality. These markers provide a permanent visual reference (unless removed during surgery) for certain procedures and for correlation with imaging across different modalities. Breast marker/clip insertion is available at NIA Imaging, performed by our highly trained Radiologists.
PURPOSE AND FUNCTION
1. Localisation for Future Imaging or Surgery
After a biopsy, a marker allows the exact location of the lesion or abnormality to be identified for follow-up, even when the lesion has resolved or is no longer visible. This is pivotal for:
Follow-up imaging such as mammography, ultrasound, or MRI Preoperative localisation prior to lumpectomy
Monitoring treatment response (e.g., post-neoadjuvant chemotherapy)
2. Treatment Planning
In cases of malignancy, markers assist surgeons and oncologists by identifying the original tumour bed, enabling accurate targeting for surgery or radiotherapy.
3. Documentation and Quality Assurance
Markers provide a permanent visual reference for radiologic–pathologic correlation and help confirm biopsy accuracy.
INDICATIONS
- Marking the location of a lesion that has been completely or almost completely removed during needle or vacuum-assisted biopsy (e.g., calcifications or small masses)
- Confirming biopsy sites when multiple lesions are present. It is recommended that a different shaped marker is used for each biopsied lesion, and this should be clearly documented during the procedure.
- Identifying the location of an ill-defined lesion.
- Assisting with future surgery or preoperative localisation when visibility is expected to be challenging, or when localisation will be performed using a different imaging modality.
- Lesion mapping for cross-modality correlation during diagnostic work-up.
TYPES OF BREAST MARKERS
1. Metallic Markers
Materials: Titanium or stainless steel (MRI-safe and biocompatible) Shapes: Various, including coil, ribbon, or butterfly designs
2. Bioabsorbable Markers
Materials: Biodegradable polymers that dissolve over time May contain a radiopaque core for long-term imaging visibility
PROCEDURE
Markers are typically inserted immediately following a core needle biopsy under ultrasound or stereotactic guidance. The marker is deployed through the biopsy needle track into the targeted site.
Post-procedure ultrasound is used to confirm the position of the marker relative to the targeted lesion (if placed under ultrasound guidance). Two-view mammography (craniocaudal and mediolateral oblique) is often performed to document final placement.
On ultrasound, the marker appears as a small echogenic focus with posterior shadowing or reverberation artefacts, depending on the material used. On mammograms, the marker appears as a small, metallic, high-density object on a mammogram, visible as a white or bright spot.
SAFETY AND PATIENT CONSIDERATIONS
Allergy check: Confirm any known allergies (e.g., nickel allergy) before selecting the marker material.
Informed consent: Must be obtained prior to the procedure.
Safety: Markers are MRI-safe (conditional) and travel-safe, posing no issues with metal detectors.
Existing Marker/Clip: Before inserting a new breast marker or clip, check whether the patient already has an existing marker at the intended site. If a marker is present, it is essential to use a clip of a different shape or design to avoid confusion on imaging and to minimise the risk of incorrect preoperative localisation during surgical excision.
POST PROCEDURE CARE
Patients are provided with a Patient Implant Information Card, which includes:
- Details of the marker or clip used
- Patient’s name and procedure date
- Name of the clinic and radiologist who performed the procedure
Patients should be advised to keep this card with them and present it to medical personnel before undergoing any future medical procedures or imaging.
Breast marker/clip insertion is available at NIA Imaging. Please call us for more information.
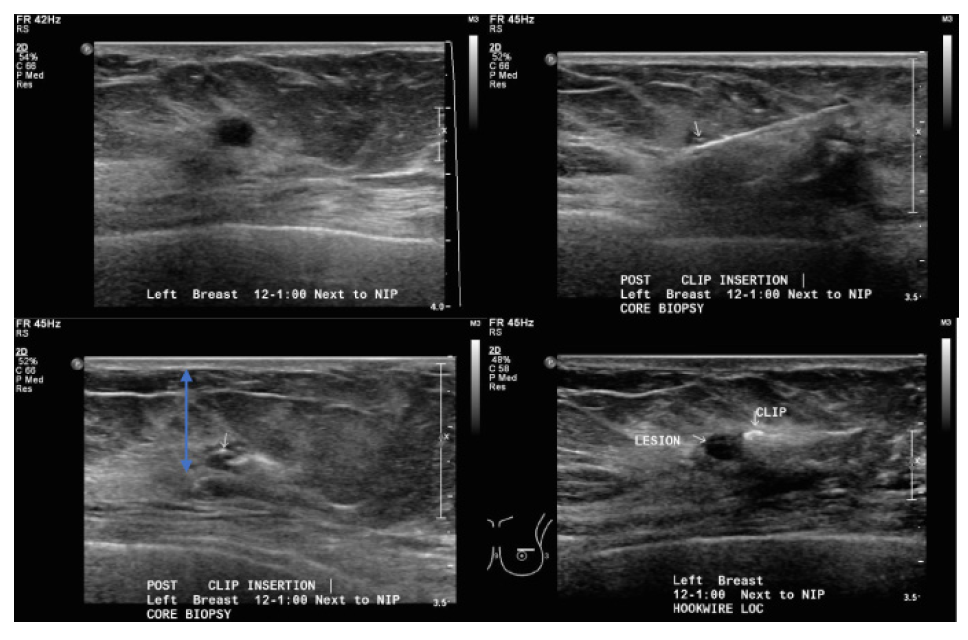
ultrasound-guided core biopsy. Small white arrow: marker.
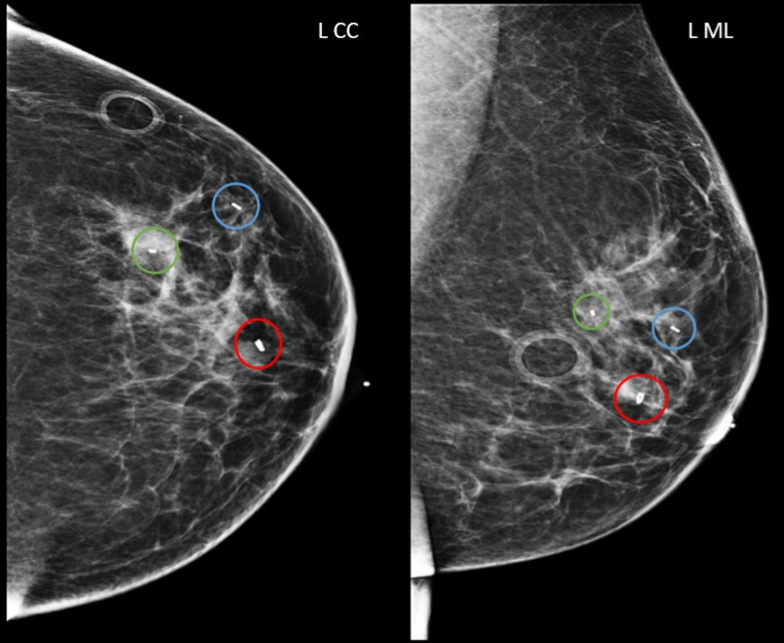
Subareolar 12 o’clock region biopsied mass with ring-shaped biopsy marker (red circles).
1 o’clock 5 cm from nipple biopsied mass with barbell-shaped biopsy marker (blue circles).
1 o’clock 6 cm from nipple biopsied calcifications with bar-shaped biopsy marker (green circles).
Craniocaudal (left image) and mediolateral (right image) views. L CC, left craniocaudal; L ML, left mediolateral
REFERENCES
- Australian Government Department of Health. (2018). Guidance for the use of marker clips by BreastScreen Australia screening and assessment services (Version 2.0). Retrieved from https://www.health.gov.au/sites/default/files/documents/2020/03/guidance-for-the-use-of-marker-clips-by-breastscreen-australia-screening-andassessment- services_0.pdf
- Breast Cancer Network Australia. (n.d.). Breast statistics: Cancer in Australia. Retrieved from https://www.bcna.org.au/resources/about-breast-cancer/breast-statisticscancer- in-australia/
- Skaane, P. (2022). Breast Imaging: A Core Review (2nd ed.). Wolters Kluwer.
- Jackman, R. J., Burbank, F., Parker, S. H., Evans, W. P., & Lechner, M. C. (2020). Tissue marker placement during breast biopsy: Techniques and clinical considerations. American Journal of Roentgenology, 214(3), 728–737.
- Mansel, R. E., Sweetland, H. M., & Kissin, M. W. (2021). Breast cancer surgery and localization: The evolving role of biopsy clips. Breast Journal, 27(5), 402–410.
- Royal College of Radiologists. (2019). Breast imaging and image-guided intervention: Guidance for practice. London: RCR.
- Lee SYS, Win T, Lee YS, Teo SY. Sonographic visibility of the UltraCorTM TwirlTM tissue marker. Breast Disease. 2022;41(1):535-543. doi:10.3233/BD-210078
- Nguyen, Quan & Tavana, Anahita & Saddrudin, Sarfaraz & Chao, Celia. (2020). Successful Lumpectomy in a Patient With Multicentric Breast Cancer. Cureus. 12. 10.7759/cureus.10072.
