20th July 2020, Dr Chee L Khoo

This is not a riddle. I often ask my medical students and patients this question and they all look at me strangely. How does this relate to medical science? Of course, we are talking about pes anserinus (PA). For those of you who remember your anatomy, PA relates to the 3 tendons that are attached to the medial aspect of the knee. Pes anserinus bursitis is not an uncommon cause of medial knee pain. This is particularly relevant in the age where everyone rushes off to have knee MRIs before an adequate knee examination. What? You have to examine the knee?
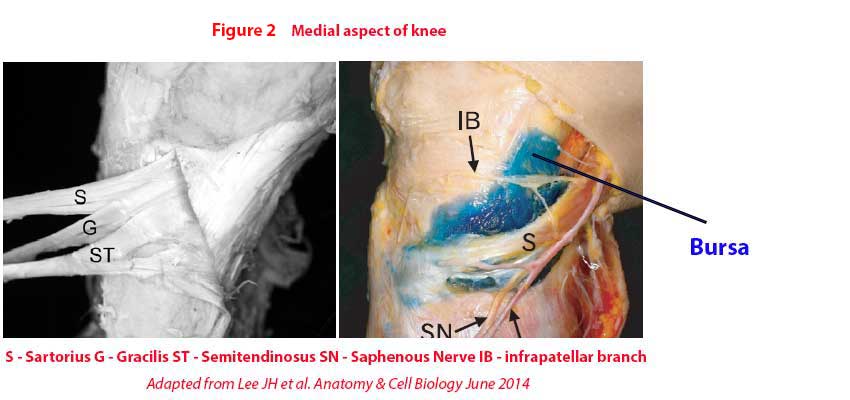
Geese have 4 “toes” but only 3 of them are on the ground (see Figure 1). The three tendons inserting at the medial aspect of the knee (generally below the joint line but not exclusively) are sartorius, gracilis and semitendinosus. The sartorius tendon is inserted in the superficial layer, and the gracilis and semitendinosus are inserted deeper on the medial surface of tibia (see Figure 2). The bursa is under the bunch of tendons (so-called pes anserinus tendon) between the tendon and the bone. The shape of the bursa is irregularly oval in shape.
PA bursitis interestingly, is more common in patients with degenerative osteoarthritis (OA) of the knee. Other predisposing factors to the development of PA bursitis are:
- Women > men
- Obesity
- Valgus genu knees
- Diabetes mellitus
When do we suspect PA bursitis?
Optimal management of knee pain is dependent upon accurate diagnosis. The standard diagnostic approach includes X-rays; however, radiographic changes may not correlate with the clinical diagnosis. It is easy for us (and the orthopaedic surgeon) to dismiss the pain as just exacerbation of OA and look no further. Intra-articular cortisone injection into the knee joint, naturally, do not reduce pain or functional symptoms and patients are then shuffled into a total knee replacement because the “cortisone injection didn’t work”.
Often, patients will complain of exacerbation of pain when going up or down stairs. Full flexion or extension also causes more pain. There is definite tenderness in the medial aspect of the knee usually, but not exclusively, below the medial joint line and not on the medial femoral condyle as one would expect in exacerbation of OA. Valgus strain does not increase the pain and this goes against a medial collateral ligament strain. Occasionally, there may be localised swelling but no effusion which makes a medial meniscal tear less likely. PA tendino-bursitis is a clinical diagnosis.
How is the diagnosis confirmed?
Well, the PA bursitis is not actually an exact science. It probably refers to a whole host of medical conditions which causes medial knee pain. Some refer to it more as pes anserinus syndrome or pes anserinus pain syndrome or anserine bursitis. Some argue that there aren’t actually any bursitis at all.
Uson et al studied the ultrasonographic features in 37 patients with the clinical diagnosis of PA tendino-bursitis syndrome (1). The painful knee was compared with the painless other knee. 93% of the patients had OA and 75% were overweight or obese. Of the 37 patients who underwent US, only one had tendonitis and two had bursitis. Thus, there weren’t many bursitis as such but more tendonitis. They defined the ultrasonographic anserine tendinitis as “presence of both thickening and loss of normal fibrillar echotexture” and bursitis as “circumscribed anechoic fluid collection of 2 mm or greater”. Hence, the term pes anserinus tendino-bursitis (PATB) was more appropriate.
PATBS is frequently associated with knee OA and vice versa. In previous studies, PATBS was clinically diagnosed in 46.8% among patients with knee OA [2]. That makes the diagnosis of medial knee pain in patients with OA that much harder, doesn’t it?
What is the management?
Well, the trick is to get the diagnosis right. Anti-inflammatory and analgesia for all knee pains irrespective of source of pain don’t cut with me because the pain will be back when you stop the medications. You need to get the diagnosis right. Physiotherapy will help if you identify the causes of the pain. That is if the physiotherapist is as switch on as you are.
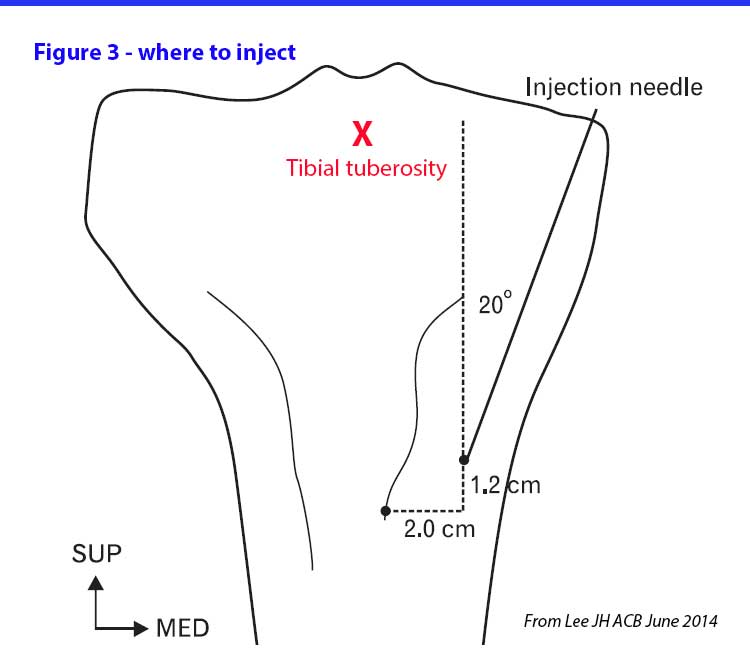
That leaves us to cortisone injections into the “bursa”. If you are referring the patient to the radiologist to have ultrasound localised injection, then you need to specifically ask for a cortisone injection into the pes anserine bursa. If you are contemplating injecting in your rooms which I sometimes do, it’s worth reading the paper by Lee YH which explains the “right” place to inject. See Figure 3.
How does the knowledge help us in clinical practice?
There are many causes of pain in the medial aspect of the knee joint. Patients with OA frequently have pes anserinus abnormalities, be it tendonitis of the pes anserinus tendon or bursitis. Not all medial knee joint pain is exacerbation of OA. A specifically targeted cortisone injection in the area of the pes anserinus can be useful treatment that can differentiate between OA or pes anserinus tendino-bursitis.
References:
- Uson J , Aguado P , Bernad M , Mayordomo L , Naredo E , Balsa A , Marto An-Mola E . Pes anserinus tendino-bursitis: what are we talking about? Scand J Rheumatol. 2000 ; 29(3) : 184 – 6
- 16. Kang I , Han SW . Anserine bursitis in patients with osteoarthritis of the knee . South Med J. 2000 ; 93(2) : 207 – 9 .
- 3. Lee, Je-Hun & Kim, Kyung-Jin & Jeong, Young-Gil & Lee, Nam-seob & Han, Seung Yun & Lee, Chang & Kim, Kyung-Yong & Han, Seung-Ho. (2014). Pes anserinus and anserine bursa: Anatomical study. Anatomy & cell biology. 47. 127-31. 10.5115/acb.2014.47.2.127.
