25th October 2020, Dr Chee L Khoo
Although our numbers of new Covid-19 infections and community transmission is pretty good in comparison with most other countries in the world, it isn’t zero. This is as good as it gets for at least the next 12 months. One of the scariest things is transmission of the virus to the newborn if the pregnant mother has the Covid-19 infection. Because the pandemic is moving so rapidly, recommendations from multiple organisations are mostly interim and can be conflicting. While these issues don’t always concern general practitioners and other non-obstetric physicians, many women will be coming to us for advice and information. So, what is the risk of mother-to-newborn transmission of Covid-19? Do we know?
Vertical transmission?
The placenta is the sole interface between the maternal and foetal environments. It protects the foetus from pathogens present in maternal blood. The maternal-foetal interface consists of foetal-derived trophoblast progenitor cells, which differentiate into cyto-trophoblasts (CTBs) and have a proliferative capacity, and syncytio-trophoblasts (STB). STB provide potent protection against both viral and nonviral pathogens. In addition, CTBs also possess innate defense mechanisms against intracellular pathogens. Strategies used by pathogens to bypass these trophoblast-intrinsic defences are varied and is beginning to be described.
The vertical transmission of infectious agents from an infected mother to her foetus can have devastating consequences in the developing foetus. Vertical transmission can be antenatal, perinatal (weeks immediately prior to or after birth), or postnatal (1).
However, studies evaluating the potential for vertical and/or postnatal transmission of Covid-19 are few in number, have small sample sizes, and come primarily from China, from which results might not generalise to all populations (2-3). Pregnant mothers who developed Covid-19 pneumonia did not fare any worse than mother who did not have Covid-19 pneumonia. There is no evidence of intrauterine infection caused by vertical transmission in women who develop COVID-19 pneumonia in late pregnancy. Outside of China, Breslin et al evaluated an initial 2 weeks of confirmed Covid-19 infection in pregnant women with similarly reassuring findings (4).
A most recent report on mothers who tested positive with Covid-19 and who presented for delivery in the first weeks of the pandemic in New York were published in the JAMA. One hundred women who delivered 101 live newborns (99 singletons and 1 twin pair) from March 13 to April 24, 2020, were included in the study. 99 women had positive test results for Covid-19 and 1 woman who presented with symptoms and chest radiographic findings consistent with COVID-19 tested negative for Covid-19 but was treated as presumptive positive. Newborns were swabbed at least once and further re-testing was performed if there were clinical symptoms or results were indeterminate.
Obstetric and Newborn Care
It is worthwhile looking at some of the details of infection prevention and control strategies (IP&C) that was developed to minimise patient-to-staff and mother-to-child transmission.
The use of personal protective equipment (PPE) was as expected. Usual obstetric care practised include delayed cord clamping, vaginal delivery (including in severe COVID-19 illness), mother-infant skin-to-skin contact, and direct breastfeeding after appropriate hand and breast hygiene (consisting of washing hands and breast with soap and water). However, all mothers, including those with COVID-19, were discharged a mean of 1 day earlier if determined to be medically and socially appropriate. All mothers received a follow-up telephone call within 48 to 72 hours of discharge.
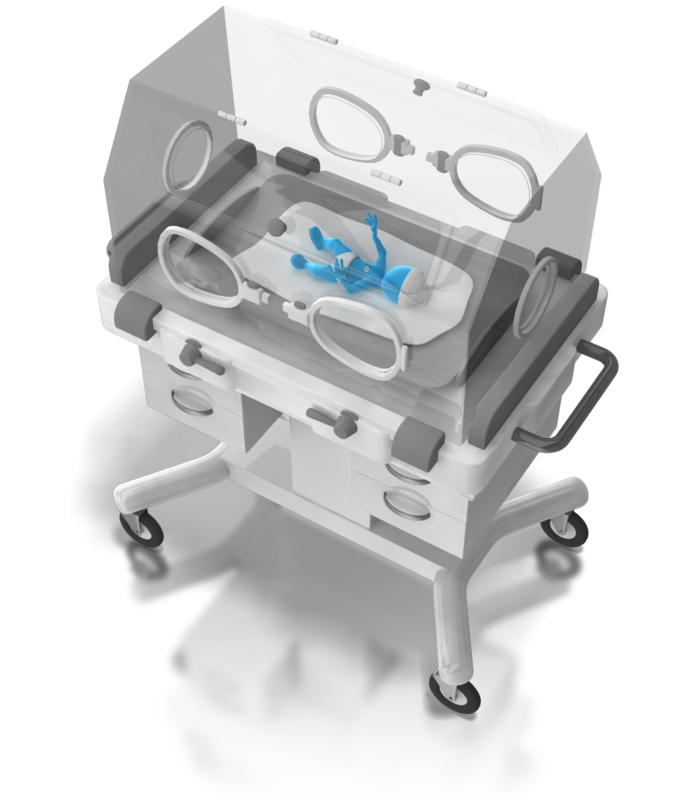
The newborns of mothers who were positive for Covid-19 were admitted to the well-baby nursery (WBN) unless they required neonatal intensive care unit (NICU) admission for standard indications. Aside from 6 mothers requiring ICU-level care, 76 mothers roomed-in with their newborns on the postpartum unit/WBN in private rooms placed on contact and droplet precautions. Newborns were in isolettes approximately 180 cm away from mothers’ beds. In the NICU, mothers positive for Covid-19 were not permitted to visit during the 14-day isolation period.
Results
The 101 neonates born to these mothers had 141 tests for Covid-19 during the study period. Seventy infants underwent testing only once. Among the newborns who underwent multiple tests, 10 tests were obtained for clinical indications, including fever and new respiratory symptoms. The remainder were obtained as part of routine additional surveillance in the NICU or COVID-19 Newborn Follow-up Clinic. Overall, incidence of transmission was 2.0% (95%CI, 0.2%-7.0%) in 2 newborns. Newborn 1 did not undergo retesting but was seen in the COVID-19 Newborn Follow-up Clinic on Day 6, and no issues were identified. Newborn 2 was born via non-emergent caesarean delivery for non-reassuring foetal heart tracing to a mother who was asymptomatic at admission but subsequently developed intrapartum fevers.16 This newborn had indeterminate test results. This newborn presented to the paediatric emergency department with excessive crying, but had normal examination results and no further testing was performed.
82 newborns (81.2%) were admitted to the WBN. 19 neonates (18.8%) were admitted to the NICU for reasons unrelated to maternal Covid-19 infection. 91 infants (90.1%; 75 in the WBN and 16 in the NICU) were born to symptomatic/mildly symptomatic mothers, and 10 (9.9%; 7 in the WBN and 3 in the NICU) were born to mothers with severe/critical COVID-19 disease. Maternal COVID-19 severity was associated with increased risk of newborn hyperbilirubinemia requiring phototherapy.
This study demonstrated that there is no evidence of vertical transmission of Covid-19 in the first 101 newborns born to mothers positive for or with suspected Covid-19 infections at a large medical centre in an epicenter of the COVID-19 pandemic. The authors ”… endorse the benefits of rooming-in, establishing breastfeeding, and delaying bathing on newborn outcomes and suggests that separating mothers positive for Covid-19 and their newborns and avoiding direct breastfeeding may not be warranted to prevent Covid-19 transmission“
That’s reassuring.
References:
- Arora N, Sadovsky Y, Dermody TS, Coyne CB. Microbial vertical transmission during human pregnancy. Cell Host Microbe. 2017;21(5):561-567. doi:10.1016/j.chom.2017.04.007
- Chen H, Guo J,Wang C, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809-815. doi:10.1016/S0140-6736(20)30360-3
- Liu D, Li L,Wu X, et al. Pregnancy and perinatal outcomes of women with coronavirus disease (COVID-19) pneumonia: a preliminary analysis. AJR Am J Roentgenol. 2020;215(1):127-132. doi:10.2214/AJR.20.23072
- Breslin N, Baptiste C, Gyamfi-Bannerman C, et al. COVID-19 infection among asymptomatic and symptomatic pregnant women: two weeks of confirmed presentations to an affiliated pair of New York City hospitals. AmJ Obstet Gynecol MFM. 2020;100118. doi:10.1016/j.ajogmf.2020.100118
- Dumitriu D, Emeruwa UN, Hanft E, et al. Outcomes of Neonates Born to Mothers With Severe Acute Respiratory Syndrome Coronavirus 2 Infection at a Large Medical Center in New York City. JAMA Pediatr. Published online October 12, 2020. doi:10.1001/jamapediatrics.2020.4298
