14th August 2021, Dr Chee L Khoo
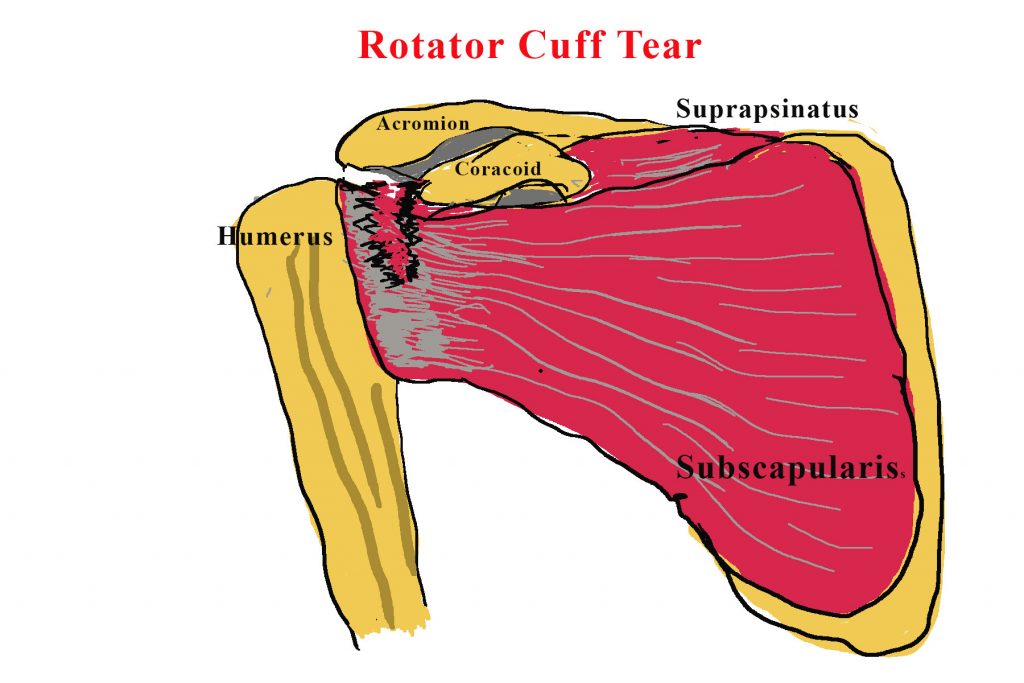
Shoulder pain has to be one of the most common musculoskeletal complaints in general practice. Rotator cuff pathology makes up at least 70% of those cases (1). It is commonly very debilitating, causing pain the whole night, causing significant reduction in function and often last for years. Apart from rest, analgesia, non-steroidal anti-inflammatory drugs, treatment options include physiotherapy, corticosteroid injections and surgical repair. Choosing the most appropriate treatment for each patient can be challenging. Results from a recent randomised controlled trial have stimulated my interest in reviewing our treatment options.
When a condition has many treatment options, it may mean the effectiveness of treatment is probably unclear. Evidence from small, short-term trials suggests that physiotherapist-prescribed exercise is promising. However, a Cochrane review highlighted widespread provision, uncertainty exists about which types of exercise and levels of physiotherapy supervision are associated with the best outcomes (2). Progressive resistance training to improve muscular strength, whether supervised or home based, has been identified as a core component of exercise for patients with rotator cuff disorders (3).
Subacromial corticosteroid injections are commonly used to reduce local tissue inflammation and pain. Remember, the aim of treatment is to improve pain and shoulder function. So, do corticosteroid injections improve pain and/or function? Corticosteroid injections have been shown to have short-term benefit in the shoulder although the longer-term benefits and harms are not known (4,5). What about combining both? Corticosteroid injections are being used increasingly in clinical practice alongside physiotherapy for the management of people with rotator cuff disorders (6).
The Getting it Right: Addressing Shoulder Pain (GRASP) trial explored the clinical effectiveness and cost-effectiveness of two interventions (7):
- individually tailored exercise program vs physiotherapy session and
- subacromial corticosteroid injection vs no injection.
Patients aged 18 years or older were recruited from 20 UK National Health Service (NHS) trusts. 708 patients who had a diagnosis of shoulder pain attributable to a rotator cuff disorder (eg, cuff tendonitis, impingement syndrome, tendinopathy, or rotator cuff tear) that had started within the past 6 months were randomly assigned in a 1:1:1:1 manner to either:
- progressive exercise
- best practice advice
- progressive exercise preceded by subacromial corticosteroid injection or
- best practice advice preceded by subacromial corticosteroid injection
Participants assigned to the progressive exercise intervention received up to six individual face-to-face sessions with a physiotherapist over 16 weeks. These sessions included a behavioural component to encourage adherence to the exercises. Exercises focused on movements commonly affected by a rotator cuff disorder: resisted external rotation, flexion, and abduction of the shoulder. Participants were given a folder containing an advice booklet, exercise action planner, diary, and instructions on their exercise programme set up in collaboration with the physiotherapist. Resistance bands were issued as required. Participants were asked to do their exercises 5 days per week, with two non-consecutive recovery days.
Participants randomly assigned to the best practice advice intervention received a single individual face-to-face session with a physiotherapist, lasting up to 60 min. Participants also received the same initial shoulder examination and advice booklet (with exercise action planner, diary, and resistance band) but the exercise programme was different. Participants were given a simple set of self-guided exercises (with access to exercise videos) that could be progressed and regressed depending on their capability. The exercises were designed using similar concepts to the progressive exercise intervention, such as increased resistance and done five times per week, but these were a simpler range of exercise options that were not supervised.
The primary outcome was shoulder pain and function over 12 months after randomisation, measured using the Shoulder Pain and Disability Index (SPADI), a 13-item measure of patient-reported outcomes in which each item is scored on a 0–10 numerical rating scale (10 being the worst score). Measurements were collected at baseline and then by postal questionnaires at 8 weeks, 6 months and 12 months after randomisation.
Results
Overall, we found a substantial improvement in SPADI score in each group over 12 months (table 3; appendix p 7). We found no evidence of a statistically significant interaction effect on the primary outcome between progressive exercise and injection over 12 months. In other words, doesn’t matter what you do, everyone got better at the end of the 12 months. We found no difference between progressive exercise and best practice advice at 8 weeks, 6 months, or 12 months.
Over 12 months, we found no evidence of a difference in SPADI scores between patients who received the injection and those who did not (adjusted mean difference –1·11 [–4·47 to 2·26]). We also found no difference between injection and no injection at 6 months and 12 months (1·93 [–2·41 to 6·27; figure 2). We found a small difference in SPADI score at 8 weeks (–5·64 [–9·93 to –1·35]), in favour of injection.
The GRASP trial demonstrated that progressive exercises (as supervised regularly by a physiotherapist) was not superior to best practice advice session with a physiotherapist. It also demonstrate that subacromial corticosteroid injection may improve short term (8 weeks) pain and function but not in the medium to long term. We can assure our patients with this chronic painful condition that relief is going to take some months and likely 1-2 years. They need to be patient with the exercise advice. In the short term, subacromial corticosteroid injection my be useful but it must be combined with ongoing exercise.
We looked at the futility of subacromial decompression surgery back in 2017 when Beard et al showed that “surgery did not appear to offer any clinically important benefit over conservative treatment of physiotherapy at 6 months and beyond” (8).
References:
- Mitchell C, Adebajo A, Hay E, Carr A. Shoulder pain: diagnosis and management in primary care. BMJ 2005; 331: 1124–28.
- Page MJ, Green S, McBain B, et al. Manual therapy and exercise for rotator cuff disease. Cochrane Database Syst Rev 2016; 6: CD012224.
- Littlewood C, Malliaras P, Chance-Larsen K. Therapeutic exercise for rotator cuff tendinopathy: a systematic review of contextual factors and prescription parameters. Int J Rehabil Res 2015; 38: 95–106.
- Buchbinder R, Green S, Youd JM. Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev 2003; 2003: CD004016.
- Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet 2010; 376: 1751–67.
- British Elbow and Shoulder Society, British Orthopaedic Association, Royal College of Surgeons. Commissioning guide: subacromial shoulder pain. 2014. https://www.rcseng.ac.uk/library-and-publications/rcs-publications/docs/subacromial-shoulder-pain/ (accessed June 21, 2021).
- Hopewell S, Keene DJ, Marian IR, Dritsaki M, et al. Progressive exercise compared with best practice advice, with or without corticosteroid injection, for the treatment of patients with rotator cuff disorders (GRASP): a multicentre, pragmatic, 2 × 2 factorial, randomised controlled trial. Lancet. 2021 Jul 31;398(10298):416-428. doi: 10.1016/S0140-6736(21)00846-1. Epub 2021 Jul 12. PMID: 34265255; PMCID: PMC8343092.
- David J Beard, Jonathan L Rees, Jonathan A Cook et al. Arthroscopic subacromial decompression for subacromial shoulder pain (CSAW): a multicentre, pragmatic, parallel group, placebo-controlled, three-group, randomised surgical trial. Lancet. First published online November 20, 2017
