14th February 2022, Dr Chee L Khoo
TOBOGM is its final stages of recruitment. TOBOGM is the very first study to see if immediate treatment of early GDM increases or reduces pregnancy complications among women with mildly higher blood glucose diagnosed before 20 weeks’ gestation. The world is waiting on the results of this landmark study. TOBOGM study results will significantly contribute to the management decision of pregnant women with early GDM. And I urgently need your help. Over the next 3 weeks, we need another 22 women who are in the early stages of pregnancy to be enrolled in the study.
Who is eligible for the study?
If a pregnant woman has any of the following risk factors:
- Previous gestational diabetes (GDM)
- Previous elevated blood glucose
- Age over 40 years
- BMI >30kg/m2
- Previous baby >4kg or 90th centile
- Parent or sibling with diabetes, or a sister with/has had GDM
- Known polycystic ovarian syndrome
- Medications: corticosteroids or antipsychotics
- Ethnicity: Non-European descent
she may be eligible for the study.
Why TOBOBM?
We all know about the harms to the mother and baby when there is hyperglycaemia during pregnancy. This is in pregnant women with type 1 or type 2 diabetes. There is:
- Perinatal mortality 4X higher than general population
- Congenital
Anomalies 2X higher than general population:
- Congenital heart disease
- Anomalies of nervous system
- Neural tube defects
- Similar between T1D & T2D
But that is with women with pre-existing diabetes and become pregnant (diabetes in pregnancy) but we also have evidence from the HAPO study that in women with lesser hyperglycaemia as in GDM, there were positive associations between increasing plasma glucose levels and both adverse maternal and offspring outcomes in a LINEAR fashion. Thus, hyperglycaemia in diabetes and GDM (diagnosed at 24-28 weeks) is associated with harm to the mother and offspring.
This is where things get a bit complicated. The HAPO study results is based on the diagnosis of GDM performed between 24-28 weeks. We cannot extrapolate these results from GDM diagnosed from fasting glucose or OGTT performed earlier than 24 weeks. There is a gap in our knowledge with treating women with early GDM whose fasting glucose is between 5.1-6.1 mmol/L. We don’t know that treatment of women diagnosed with slightly high glucose in early pregnancy is beneficial or even safe for both mother offspring. This is what TOBOGM is seeking to find out. The whole world is anxiously waiting for answers to this question.
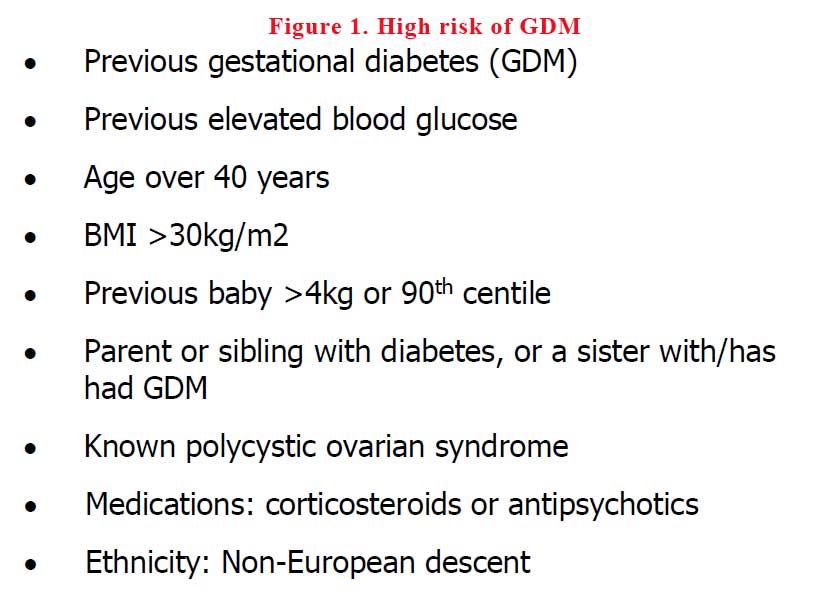
So, if you have women who are pregnant and are at risk (see Figure 1) of developing GDM, please do not organise an OGTT. Refer them to TOBOGM by emailing to ToBOGM@westernsydney.edu.au before they have their OGTT. They will be randomised and closely monitored to either treatment or no treatment groups (See Figure 2).
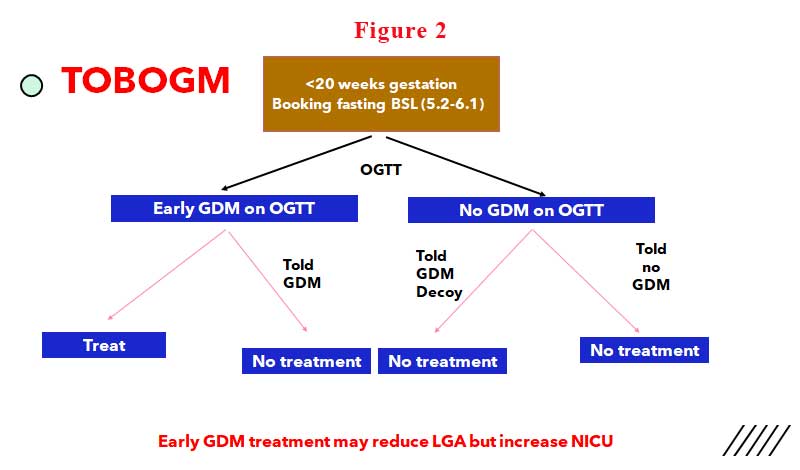
Remember, does your patient need treatment? Are you doing any harm to her or her baby by instituting treatment for GDM when neither mother or baby derived benefit from low carb low sugar diets?
You can download the TOBOGM brochure here.
