5th January, 2019, Dr Chee L Khoo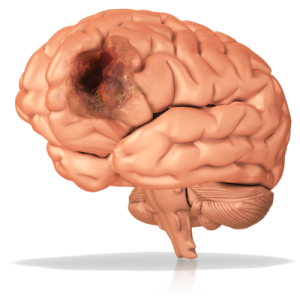
The incidence of ischaemic strokes in young adults is on the increase. Worldwide, it has risen up to 40% over the past decades. This contrasts with the decreasing incidence of stroke in older adults. It’s never a good time to have a stroke whatever the age of onset is but the socioeconomic costs are much higher in the younger. Investigating the causes and risk factors in the young stroke victim is very different from investigating an older stroke victim.
There is no formal consensus in what is defined as “young” although most studies define this population as between 18 – 50 years old. Unfortunately, young adults are often under-represented in clinical studies even though the prevalence of the traditional risk factors among our young adults is increasing. Further, young adults are at a much higher risk of recurrent stroke and mortality than their healthier peers. Recommendations from most international guidelines are extrapolated from older adults with strokes.
One of the more widely used classification of strokes (including strokes in young adults) is the TOAST classification (1):
|
TABLE 1. TOAST Classification of Subtypes of Acute Ischemic Stroke |
| Large-artery atherosclerosis (embolus/thrombosis) |
| Cardioembolism (high-risk/medium-risk) |
| Small-vessel occlusion (lacune) |
| Stroke of other determined etiology |
| Stroke of undetermined etiology
a. Two or more causes identified b. Negative evaluation c. Incomplete evaluation |
Large artery atherosclerosis
The traditional risk factors giving rise to atherosclerotic events are similar in young and old adults although the population-based attributable risks of smoking, waist-to-hip ratio, alcohol intake, and psychosocial factors are slightly higher in young adults with stroke compared with old patients (2). These traditional risk factors combined accounted for almost 80% of all ischaemic strokes in young adults (3). The increasing problems relating to the diabesity epidemic will see large artery atherosclerosis becoming a bigger problem in young adults in the foreseeable future.
Cardioembolism
Atrial fibrillation is high on the list of conditions to exclude even in young adults with an acute ischaemic stroke. Patent foramen ovale (PFO) is increasingly being diagnosed in young adults with an ischaemic stroke as our index of suspicion becomes higher and we have better investigations available. We covered PFO as part of the investigations for embolic strokes of undetermined source (ESUS) in the last issue.
Other sources of cardioembolism are endocarditis with or without valve vegetations, cardiomyopathy and cardiac tumours.
Small vessel disease
These are cerebral small vessel diseases presenting as ischaemic strokes in young adults. MRI or CT shows up multiple white matter hyperintensities, microbleeds and lacunae. Naturally, if there are traditional risk factors, they need aggressive management. Long term anti-platelet therapy is recommended.
There is a small subset of these patients that may have cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL). CADASIL is the most common form of hereditary cerebral angiopathy with typical MRI images of widespread white matter hyperintensities, subcortical infarcts (including external capsule infarcts) and microbleeding.
CADASIL may start with attacks of migraine with aura or subcortical transient ischemic attacks or strokes, or mood disorders between 35 and 55 years of age. The disease progresses to subcortical dementia associated with pseudobulbar palsy and urinary incontinence.
CADASIL is caused by a mutation in the NOTCH3 gene on chromosome 19q12. The gene codes for a membrne protein receptor whose function is unknown. The mutant receptor protein accumulates in small and medium sized arteries (including cerebral) causing fibrosis of the walls. See here for more features of CADASIL.
Stroke of other determined cause
These encompasses a long list of diseases with known complications of ischaemic strokes:
- Anti-phospholipid syndrome – covered few issues back
- Fabry disease
- Clotting disorders including Factor II Deficiency, Factor V Leiden, Protein C deficiency.
- Vasculitis
- Illicit drug use
- Malignancies
- Post radiation
- Cervical artery dissection
- Reversible cerebral vasoconstriction syndrome
Stroke of undetermined causes
These are labelled as cryptogenic strokes.
Although there are significant differences in causes and risk factors between young and older adults with ischaemic stroke, a significant proportion of the strokes in the young adult is still associated with the traditional risk factors. But if we come across a patient whose atherosclerotic burden doesn’t quite explain the cause of the stroke, we need to look further.
References:
- Adams HP, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993; 24: 35–
- O’Donnell MJ, Chin SL, Rangarajan S, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet 2016; 388: 761–
- Aigner A, Grittner U, Rolfs A, Norrving B, Siegerink B, Busch MA. Contribution of established stroke risk factors to the burden of stroke in young adults. Stroke 2017; 48: 1744–
- Merel S Ekker*, Esther M Boot*, Aneesh B Singhal, Epidemiology, aetiology, and management of ischaemic stroke in young adults. Lancet Neurol 2018; 17: 790–801
