8th June 2019, Dr Chee L Khoo
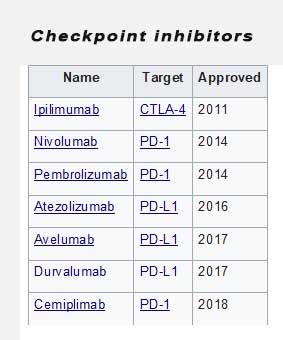
Checkpoint inhibitors are monoclonal antibodies that block checkpoint molecules, cytotoxic T-lymphocyte-associated protein 4 (CTLA-4), programmed death-1 (PD-1) and PD-1 ligand 1 (PD – L1). They have revolutionised cancer treatment because of their ability to improve survival in a growing number of cancers. Some of the cancers that have been successfully treated include melanoma, lung cancer, kidney cancer, bladder cancer, head and neck cancer, and Hodgkin’s lymphoma. A new form of insulin-dependent diabetes has been recognised, occurring in patients with cancers who are treated with checkpoint inhibitors.
Checkpoint molecules are key regulators of the immune system. These checkpoint molecules are expressed by T cells and are essential for maintenance of immunological tolerance by preventing the unimpeded activation of T cells. CTLA-4 plays an important part in the inhibition of early T-cell responses and in T regulatory cell function, whereas the interaction of PD-1 with its ligands PD-L1 and PD-L2 inhibits effector T cells in peripheral tissues and promotes T-cell exhaustion. Tumour cells capitalise on these checkpoint molecules to protect themselves from attacks by the immune system. Checkpoint therapy block inhibitory checkpoints, restoring immune system function.
But there is no free lunch. Checkpoint inhibitors (CPIs) can also result in immune-related adverse events that affect various organ systems including endocrine organs like the pituitary gland, thyroid gland, adrenal glands, and the insulin-producing β cells of the pancreas. In a review of the literature, Heinzerling cited the most common are skin lesions (46–62%), autoimmune colitis, (22–48%), autoimmune hepatitis (7–33%), and endocrinopathies (thyroiditis, hypophysitis, adrenalitis, diabetes mellitus; 12–34%) (1). Rarer side effects include pneumonitis (3–8%), nephritis (1–7%), cardiac side effects including cardio-myositis (5%), and neurological side effects (1–5%).
Checkpoint inhibitors-induced type 1 diabetes (CIID)
Checkpoint inhibitor-induced diabetes represents a new-onset insulin-dependent diabetes, which is often acute, following the treatment of a malignancy with checkpoint inhibitors. Checkpoint inhibitor-induced diabetes most commonly occurs following treatment with anti-PD-1 or anti PD-L1 monoclonal antibodies, alone or in combination with anti-CTLA-4 monoclonal antibody, but two studies (2,3) have described cases in which insulin-dependent diabetes occurred after anti-CTLA-4 monoclonal antibody treatment alone.
CIID has been reported in about 1% of patients treated with CPIs but as the use of these agents increases, we can expect can expect the incidence of CIID to increase. It has been reported most frequently in patients with malignant melanoma probably because CPIs were initially trialled on these patients. It has been reported in at least 13 other malignancies treated with CPIs. It is unclear whether these patients had pre-existing auto-immune disease.
The clinical onset of CIID is typically acute (like the usual type 1 diabetes ) with markedly high blood glucose levels. The median time of onset from the initiation of CPIs is about 11 weeks. Diabetes ketoacidosis was seen in 75% of patients and C-peptide levels were either below normal or undetectable in 91% of the patients. Most studies have only analysed the anti-GAD antibodies which was present in 48% of patients. The frequency of other auto-antibodies seen in type 1 diabetes (T1DM) is unknown at this stage. Patients with anti-GAD antibodies had a shorter interval from initiation of CPIs to CIID (7 weeks vs 11 weeks). Perhaps, these were latent T1D.
CIID appears to be similar to full on T1DM. Insulin therapy is needed in almost all patients with CIID. The glucose control is typically labile with higher frequency of severe hypoglycaemia and ketoacidosis. Understanding the pathogenesis of CIID may help us identify who is at higher risk of these endocrine adverse events. Further studies are needed to determine whether non-insulin-requiring patients with type 2 diabetes who develop substantial worsening of their disease might also have a mild form of this immune-related adverse event, since insulin production is not eliminated entirely. Understanding the role of checkpoint molecules in the destruction of beta cells may open up therapeutic avenues in the management of diabetes, both T1DM and T2DM.
It is important that, as GPs we need to be aware of this new syndrome as patients may be presenting to us at the practice in between their visits to the oncologist. Although the incidence of CIID is still low (1%), should patient be warned of this potential adverse events when they are considering their anti-cancer therapeutic options.
References:
- Heinzerling L, de Toni E, Schett G, Hundorfean G, Zimmer L: Checkpoint inhibitors—the diagnosis and treatment of side effects. Dtsch Arztebl Int 2019; 116: 119–26. DOI: 10.3238/arztebl.2019.0119
- Wright JJ, Salem JE, Johnson DB, et al. Increased reporting of immune checkpoint inhibitor-associated diabetes. Diabetes Care 2018; 41: e150–
- Yamazaki N, Kiyohara Y, Uhara H, et al. Phase 2 study of ipilimumab monotherapy in Japanese patients with advanced melanoma. Cancer Chemother Pharmacol 2015; 76: 997–
- Kotwal A, Haddox C, Block M, et al. Immune checkpoint inhibitors: an emerging cause of insulindependent diabetes. BMJ Open Diab Res Care 2019;7:e000591. doi:10.1136/bmjdrc-2018-000591
- Venetsanaki, A. Boutis, A. Chrisoulidou, P. Papakotoulas. Diabetes mellitus secondary to treatment with immune checkpoint inhibitors. Curr Oncol. 2019 Feb;26(1):e111-e114
