27th May 2023, Dr Chee L Khoo
The first GLP1- RA, exenatide was first isolated by John Eng in 1992 while working at the Veterans Administration Medical Center in the Bronx, New York.[1] It was made by Amylin Pharmaceuticals and commercialised by AstraZeneca. Exenatide was approved by the FDA on April 28, 2005, for people whose diabetes is not well controlled on other oral medications. Since then, there has been increasing number of “better” GLP1-RAs being developed. Of course, we started with short acting exenatide which needs to be administered twice a day. We then have the longer acting once a day liraglutide (Victoza, Saxenda) and Lixisenatide (not available in Australia). We now have the even longer acting, weekly GLP1-RAs, semaglutide, dulaglutide and abiglutide (not available anywhere). We also have oral semaglutide. There is a new kid on the block – oral danuglipron.
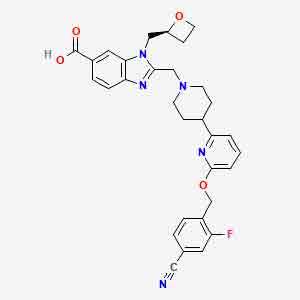
The GLP-1 receptor is a seven-transmembrane-spanning, class B, G protein-coupled receptor (GPCR). Class B GPCRs can be activated by either endogenous peptide hormones (i.e GLP1-RA) or non-peptide ligands. However, the development of small-molecule non-peptide agonists of the GPCR has proven to be particularly challenging. Danuglipron was developed in an attempt to obtain a small-molecule oral GLP1-RA that could be used in standard formulations and could therefore be combined with other oral therapies, unlike oral semaglutide.
How efficacious is danuglipron in reducing glycaemia in patients with T2D and in weight loss?
A phase I study conducted to assess the safety profile, pharmacokinetics, and pharmacodynamics of the drug showed that HbA1c was reduced by 0.9%, 1.2%, and 1.2% at doses of 15, 70, and 120 mg, respectively, and that body weight was decreased by 4.0 kg (70 mg dose) and 7.9 kg (120 mg dose) after 4 weeks of treatment. The safety profile and tolerability of danuglipron were found to be similar to other GLP1Ras (2).
In the latest Phase 2b multicentre double-blind, placebo-controlled trials, adults with T2D inadequately controlled by diet and exercise, with or without metformin treatment, were enrolled and randomised to 6 parallel groups (2.5, 10, 40, 80, or 120 mg twice daily or placebo) (3).
Reductions in HbA1c and FPG, compared with placebo, were evident for all danuglipron groups as early as week 2 and continued through week 16, with some exceptions for the lowest-dose group. Reductions in HbA1c at week 16 were relatively similar across danuglipron doses of 10 to 120 mg twice daily. A greater proportion of participants receiving danuglipron compared with placebo achieved the glycaemic target of HbA1c less than 7%, and the proportion achieving this target generally increased with higher danuglipron doses.
Body weight was statistically significantly reduced at week 16 compared with placebo in the 80-mg twice daily and 120-mg twice daily groups only, with a least squares mean difference vs placebo of −2.04 kg for the 80-mg twice daily group and −4.17 kg for the 120-mg twice daily group.
The weight loss with danuglipron in this study is of a similar magnitude to that observed in the phase 2 data for oral semaglutide and the injectable GLP-1R agonists during similar durations of dosing (13-15).
The most common adverse events were gastrointestinal in nature and consisted of nausea, diarrhea, and vomiting. Most adverse events with danuglipron were mild, although they were also the most common reason for discontinuation. The discontinuations were dose responsive.
Injectable GLP-1RA are approved for the treatment of type 2 diabetes mellitus (T2D) and for the treatment of obesity. Excitement has grown in this drug class, with several GLP-1R agonists demonstrating benefit in cardiovascular outcome studies. A drawback of these medicines has been the necessity to administer them via subcutaneous injection, which limits patient utilisation and may reduce opportunities for fixed dose combination treatments with other small-molecule therapies for cardio-metabolic diseases. Further, injectables are harder to manufacture and their injectable devices takes additional time for approval by regulatory authorities. Hence, the worldwide shortages we are so familiar with.
It’s a new, albeit smaller, kid on the GLP-1 RA block. It seems to be as efficacious in glucose lowering and weight reduction as oral semaglutide. It might arrive at our shores faster than you think.
References:
- Raufman JP (January 1996). “Bioactive peptides from lizard venoms”. Regulatory Peptides. 61 (1): 1–18. doi:10.1016/0167-0115(96)00135-8.
- Saxena AR, Gorman DN, Esquejo RM, Bergman A, Chidsey K, Buckeridge C, Griffith DA, Kim AM. Danuglipron (PF-06882961) in type 2 diabetes: a randomized, placebo-controlled, multiple ascending-dose phase 1 trial. Nat Med. 2021 Jun;27(6):1079-1087. doi: 10.1038/s41591-021-01391-w.
- Saxena AR, Frias JP, Brown LS, et al. Efficacy and Safety of Oral Small Molecule Glucagon-Like Peptide 1 Receptor Agonist Danuglipron for Glycemic Control Among Patients With Type 2 Diabetes: A Randomized Clinical Trial. JAMA Netw Open. 2023;6(5):e2314493. doi:10.1001/jamanetworkopen.2023.14493
