10th June 2024, A/Prof Chee L Khoo
Identification of individuals at high risk of atherosclerotic cardiovascular events is actually quite challenging in practice. There are many predictive algorithms which try to assess the cardiovascular risk of an individual. These scoring systems are based on the traditional risk factors that we all know well – lipids, smoking, hypertension, diabetes, family history of atherosclerotic cardiovascular disease (ASCVD), age and gender but unfortunately, we still don’t fully understand an individual’s susceptibility to the atherogenic vulnerability. Clinical risk estimates have proven to be a poor predictor of the actual burden of coronary atherosclerosis (1). The various scoring systems may work well on a population basis but predicting events for the patient sitting in front of you is not that great. What can help us predict with better accuracy?
We often resort to organising a stress test, whether stress echocardiography or nuclear stress testing, to see whether there is/are flow limiting coronary artery stenosis in both our symptomatic or asymptomatic patients. When the results come back as negative, we might breathe a sigh of relief but we forget about the limitation of a functional test.
A stress test is designed to test the dynamic flow adequacy of the coronary circulation with the aim to determine whether there are critical stenoses of the coronary circulation mandating either a revascularisation procedure (percutaneous coronary intervention or bypass surgery) or medical treatment for ischaemia. A negative stress test means there are unlikely to be any stenoses > 75%. There are occasions where there may be stenoses > 90% but the patient’s system has adapted to the flow limitation and the functional stress test can still be negative.
A negative stress test definitely do not assess for the atherosclerotic burden of disease which is vital in determining the aggressiveness of the management of the risk factors, in particular, LDL-C. While stenosis between 50-75% does not require revascularisation, it is considered “established” cardiovascular disease and there are significant differences in management targets as established cardiovascular disease demands aggressive treatment of the risk factors irrespective of whether an event or revascularisation has occurred.
In practice, the majority of events occurs in patients with normal stress testing, highlighting the importance of detecting non-obstructive CAD for more effective prevention of major adverse cardiovascular events (MACE) (2). The inability to detect high-risk atherosclerosis is highlighted further by fact that many patients experience out-of-hospital sudden cardiac death as their first and final cardiovascular event (3). Many individuals develop ASCVD, plaque rupture, and myocardial infarction without a single standard modifiable risk factor reaching the threshold for ‘action’ (4-8). A negative stress test therefore can provide a false sense of security that all is good.
When we try to personalise the CV risk assessment of the patient sitting in front of us, we may need other additional information. While the various CV scores can sometimes surprise us with a higher scores than anticipated, often, they underestimate the patient’s CV risk. The Australian CVD risk calculator allows us to add to the estimated risk if the patient have other additional risk factors not required for the calculator. An elevated lipoprotein (a) level or family history of familial hypercholesterolaemia (FH) or the presence of other atherogenic co-morbidities (e.g fatty liver disease) may warrant an upgrade of the estimated risk scores.
Further imaging?
A coronary artery calcium score (CAC) may be a useful and relatively cheap way of further clarifying the CV risk in patients whom we suspect may have higher CV risks than what the scores tell us. However, a low score (<100) may not exclude the presence of soft plaques. Further, a high score may indicate stable calcified plaques which may mitigate a high CAC score. CAC data from population-based studies have revealed up to 1 in 4 younger individuals who will suffer MACE will have a CACS = 0 at the time of imaging (2,9).
Benefits of CCTA
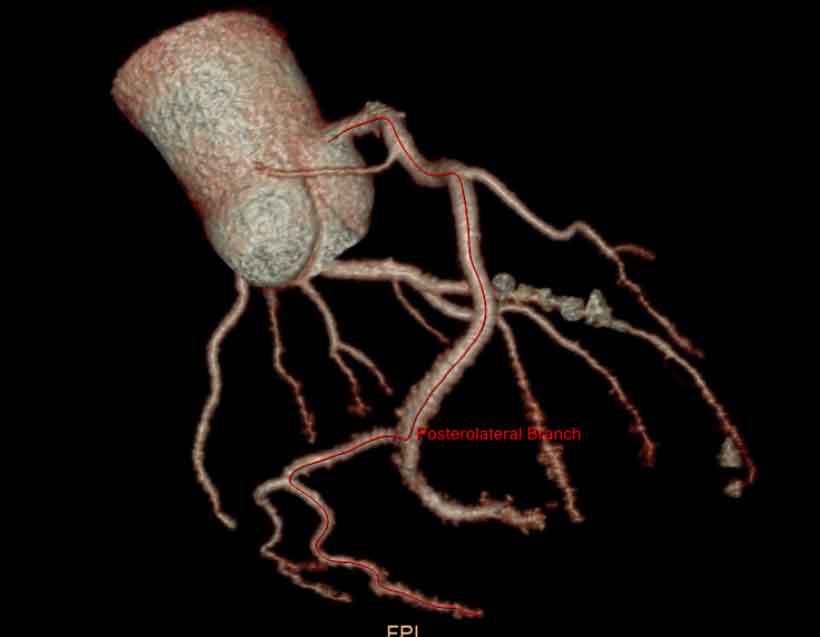
Over the last 20 years, CT scanners and techniques for CCTA have substantially improved. The current 3rd-generation, CT scanners can achieve a maximum spatial resolution of 0.24 mm and a temporal resolution up to 66 ms while drastically reduced the average radiation dose to below 3 mSv which is equivalent to the amount of annual exposure due to background radiation for an individual living at sea level (10). Corballis N et al found no difference in MACE between CCTA and invasive angiogram as a first line investigation for stable angina (11). CCTA when compared to intravascular ultrasound (IVUS), showed a sensitivity and specificity of 93% and 92%, respectively (12).
Diameter stenosis, plaque burden, and specific plaque phenotypes, such as non-calcified and, in particular, low-attenuation plaque, are considered some of the most potent markers for future MACE and carry the potential to be the standard of care for risk assessment. CCTA offers the ability to quantify plaque burden and assess plaque morphology, as well as the ability to define high-risk measures of plaque and vascular morphology.
Lack of MBS re-imbursement – why
Historically, the reason to perform functional stress testing was to determine whether any intervention is necessary. There are no mortality or survival benefits of revascularisation and intervention was meant to be for symptom control which means, in patients who are asymptomatic, since there are no mortality benefit, medical treatment is as good as intervention (13-17).
Thus, one would not need to know whether there are any lesions <75% if there are no symptoms since the management is the same. That’s the rationale why the Medicare Benefits Schedule (MBS) says that since you are not going to change your management in patients with negative stress test and are asymptomatic, you need not perform an angiogram. Angiogram was used to treat stenosis and not treat atherosclerosis.
The UK National Institute for Health and Clinical Excellence (NICE) no longer recommend the use of pretest probability risk scores and it has removed functional tests, such as stress echocardiography, as first-line investigation in patients with new onset stable chest pain. It recommends using CT coronary angiography in the majority of patients (18). The European Society of Echocardiography recommends CTCA or functional ischaemic testing to be considered depending on patient characteristics and preference, availability and local experience (19). The American Heart Association (AHA)/ American College of Cardiology (ACC) have recommended either CTCA or functional testing to investigate patients with stable chest pain and an intermediate-high risk of coronary disease (20).
Studies showing benefit
Functional testing only report on the adequacy of flow while CCTA reports on the extent of coronary artery disease. Compared with a normal CCTA, the presence of angiographically non-obstructive, one-vessel obstructive, two-vessel obstructive, and three-vessel or left main obstructive CAD were 2.2X, 2.9X, 3.5X, and 4.7X for myocardial infarction or death (21). In other words, the degree of stenosis is not as important as the diffuseness of the atherosclerosis.
Why does it matter?
In addition to statins and ezetimibe which have been convincingly shown to reduce CV events, we now have a whole array of agents, some novel and some old that target different components of the atherosclerotic process. This include the SGLT2 inhibitors, the PSCK9 inhibitors and inclisiran, GLP1-RA, bempedoic acid and colchcine.
While older studies did not show any mortality benefit with revascularisation, the SCOT-HEART trial showed that in patients with stable chest pain, CCTA-guided care, which resulted in a 40% reduction in death from CHD or myocardial infarction at 5-year follow-up compared with standard care (22). The direct visualisation of atherosclerosis by CCTA led to higher rates of statin and aspirin prescription, and more appropriate prescriptions targeting patient with actual disease, which can explain the benefit observed in SCOT-HEART (23,24).
Finally, studies such HUYGENS, PACMAN-AMI and GLAGOV demonstrated that aggressive reduction in LDL-C can result in reduction of the atherosclerotic plaque volume, increase in fibrous cap thickness and reduction in lipid content in the lipid-rich plaque, all of which reduces MACE (25-27). We now have the means to reduce plaque volume and increase plaque stability by aggressively reducing LDL-C in patients with or without established coronary artery disease.
These new developments have shifted our management from ischaemia focus to atherosclerosis prevention focus. It also shifts our paradigm from population based risk factor prevention strategy to a personalised disease burden based prevention strategy.
In summary, while functional stress testing remains a common way to determine whether our at-risk patients have significant coronary artery stenosis, there are limitations in what it can safely exclude. The original intent of stress testing was to find patients that need revascularisation but the management paradigm back then was stenosis and symptomatic management rather than atherosclerosis management. Recent studies have demonstrated that aggressive LDL-C lowering can lead to plaque regression and plaque stabilisation. Although mortality outcomes from the aggressive lipid management has yet to be established, it is time that we re look at which of our patients need further clarification with a CCTA and which of our patients need more aggressive lipid lowering. Functional stress testing can’t tell us that. Currently, there is no MBS rebate for a CCTA in patients who are asymptomatic but it may be a small price to pay for some of our patients.
Unfortunately, our data is incomplete. Longer duration randomised controlled trials with larger sample sizes are pending but it’s a few more years before they report (SCOT-HEART2 – 2029, DANE-HEART – 2033, TRANSFORM – 2029). In the meantime, we will need to individualise our CV risk assessment.
References:
- Rana JS, Dunning A, Achenbach S, et al. Differences in prevalence, extent, severity, and prognosis of coronary artery disease among patients with and without diabetes undergoing coronary computed tomography angiography: results from 10,110 individuals from the CONFIRM (Coronary CT Angiography Evaluation For Clinical Outcomes): an InteRnational Multicenter Registry. Diabetes Care 2012;35:1787–94.
- Budoff MJ, Mayrhofer T, Ferencik M, et al. Prognostic value of coronary artery calcium in the PROMISE study (Prospective Multicenter Imaging Study for Evaluation of Chest Pain). Circulation 2017;136:1993–2005
- Cavallari I, Bhatt DL, Steg PG, et al. Causes and risk factors for death in diabetes: a competing-risk analysis from the SAVOR-TIMI 53 trial. J Am Coll Cardiol 2021;77:1837–40.
- Vernon ST, Coffey S, Bhindi R, et al. Increasing proportion of ST elevation myocardial infarction patients with coronary atherosclerosis poorly explained by standard modifiable risk factors. Eur J Prev Cardiol 2017;24:1824–30
- Figtree GA, Vernon ST, Hadziosmanovic N, et al. Mortality in STEMI patients without standard modifiable risk factors: a sex disaggregated analysis of SWEDEHEART registry data. Lancet 2021;397:1085–94.
- Figtree GA, Vernon ST, Harmer JA, et al. Clinical pathway for coronary atherosclerosis in patients without conventional modifiable risk factors: JACC State-of-the-Art Review. J Am Coll Cardiol 2023;82:1343–59.
- Kelly C, Lan NSR, Phan J, et al. Characteristics and outcomes of young patients with ST-elevation myocardial infarction without standard modifiable risk factors. Am J Cardiol 2023;202:81–9.
- Kong G, Chin YH, Chong B, et al. Higher mortality in acute coronary syndrome patients without standard modifiable risk factors: results from a global meta-analysis of 1,285,722 patients. Int J Cardiol 2023;371:432–40.
- Hussain A, Ballantyne CM, Nambi V. Zero coronary artery calcium score: desirable, but enough? Circulation 2020;142:917–9.
- Seppelt D, Kolb C, Kühn JP, Speiser U, Radosa CG, Hoberück S, et al. Comparison of sequential and high-pitch-spiral coronary CT-angiography: image quality and radiation exposure. Int J Cardiovasc Imaging 2019;35:1379–86.
- Corballis N, Tsampasian V, Merinopoulis I, et al. CT angiography compared to invasive angiography for stable coronary disease as predictors of major adverse cardiovascular events- A systematic review and meta-analysis. Heart Lung. 2023 Jan-Feb;57:207-213.
- Fischer C, Hulten E, Belur P, et al. Coronary CT angiography versus intravascular ultrasound for estimation of coronary stenosis and atherosclerotic plaque burden: a meta-analysis. J Cardiovasc Comput Tomogr 2013;7:256–66.
- 3. Moss AJ, Williams MC, Newby DE, Nicol ED. The Updated NICE Guidelines: Cardiac CT as the First-Line Test for Coronary Artery Disease. Curr Cardiovasc Imaging Rep. 2017;10(5):15. doi: 10.1007/s12410-017-9412-6. Epub 2017 Mar 27.
- Boden WE, O’Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356:1503–16.
- Frye RL, August P, Brooks MM, et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med 2009;360:2503–15.
- Al-Lamee R, Thompson D, Dehbi HM, et al. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet 2018;391:31–40.
- Maron DJ, Hochman JS, Reynolds HR, et al. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med 2020; 382:1395–407
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Circulation 2019;140:e596–646.
- Juhani Knuuti, William Wijns, Antti Saraste, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes: The Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC), European Heart Journal, Volume 41, Issue 3, 14 January 2020, Pages 407–477
- Martha Gulati M.M.F.F. Phillip D. et al. AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: a Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021
- Schulman-Marcus J, Hartaigh BÓ, Gransar H, Lin F, Valenti V, Cho I, et al. Sex-Specific associations between coronary artery plaque extent and risk of major adverse cardiovascular events the CONFIRM long-term registry. JACC Cardiovasc Imaging 2016;9: 364–72
- Newby DE, Adamson PD, Berry C, et al. Coronary CT angiography and 5-year risk of myocardial infarction. N Engl J Med 2018;379:924–33.
- Adamson PD, Williams MC, et al. Guiding therapy by coronary CT angiography improves outcomes in patients with stable chest pain. J Am Coll Cardiol 2019;74:2058–70.
- Blankstein R, Bittencourt MS, Bhatt DL. Coronary CTA in the evaluation of stable chest pain: clear benefits, but not for all. J Am Coll Cardiol 2017;69:1771–3.
- Nicholls SJ, Kataoka Y, Nissen SE, et al. Effect of Evolocumab on Coronary Plaque Phenotype and Burden in Statin-Treated Patients Following Myocardial Infarction. JACC Cardiovasc Imaging. 2022 Jul;15(7):1308-1321.
- Räber L, Ueki Y, Otsuka T, et al; PACMAN-AMI collaborators. Effect of Alirocumab Added to High-Intensity Statin Therapy on Coronary Atherosclerosis in Patients With Acute Myocardial Infarction: The PACMAN-AMI Randomized Clinical Trial. JAMA. 2022 May 10;327(18):1771-1781
- Nicholls SJ, Puri R, Anderson T, Ballantyne CM, et al. Effect of Evolocumab on Progression of Coronary Disease in Statin-Treated Patients: The GLAGOV Randomized Clinical Trial. JAMA. 2016 Dec 13;316(22):2373-2384.
