23rd March 2019, Dr Chee L Khoo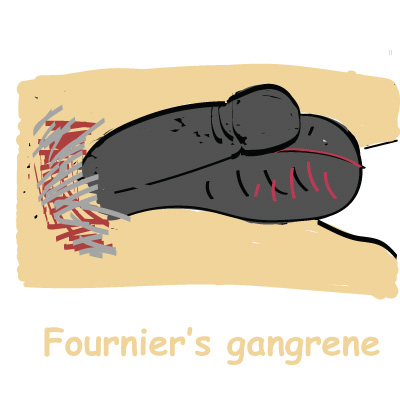
You may remember receiving warnings recently from the Therapeutics Goods Administration (TGA) about a serious “rare” infection, called necrotising fasciitis of the perineum, also referred to as Fournier’s gangrene (FG). FG is reported to be associated with the use of SGLT2 inhibitors in patients with type 2 diabetes (T2D). The warning came on the back of similar warnings by the US Food and Drug Authority (FDA) in August 2018. So, what is FG? Who are at risk? How rare is “rare”? How do they present in general practice?
FG was named after Dr Jean Alfred Fournier who was the chair of dermatology and syphilology at Saint Louis Hospital, Paris from 1880 to 1902 (1-3). Dr Fournier’s reported 5 cases of infective necrotising fasciitis of the external genitalia, perineal or perianal regions. He certainly wasn’t the first to report on genital gangrene. Between 1763 and 1978, the literature contained 386 cases of Fournier gangrene.
Bacteraemia is considered a starting link in the mechanism of the development of necrosis of the fascia that initiates the cytokine cascade leading to the damage of the endothelium, which in turn activates by means of thromboplastin, a coagulation cascade with inhibition of fibrinolysis and the formation of disseminated micro-thrombosis of vessels feeding the fascia. In addition, damage to the endothelium leads to extravasation of the liquid part of the blood, swelling of tissues, leukocyte infiltration, all leading to the ischemic necrosis of the fascia.
Local signs include ulceration in the glans penis, prepuce, skin of the penis, or scrotum. Within a few hours, the genitalia hyperaemia increases and tissue necrosis occurs. The progression of infection can lead to systemic symptoms, sepsis, multi-organ failure and death. Mortality rate can be as high as 90%. A delay of even a few hours from suspicion of FG to surgical debridement significantly increases the risk of death (4).
The differential diagnosis of Fournier gangrene includes scrotal and perineal disorders, as well as intra-abdominal disorders such as cellulitis, abscess, strangulated hernia, pyoderma gangrenosum, allergic vasculitis and vascular occlusion syndromes.
Older patients, T2D, morbid obesity, cardiovascular disorders, chronic alcoholism, long-term corticosteroid treatment, malignancy, and human immunodeficiency virus infection, urethral obstruction, instrumentation, urinary extravasation, and trauma have also been associated with this condition. The average age of patients is 50.9 years and the ratio of men to women is 10:1 (5).
Early recognition of the symptoms and signs is vital. The basis of therapy for FG is emergency surgical intervention in combination with antibacterial and detoxification therapy. Reconstructive surgical treatment is performed after the formation of granulation tissue. It includes complex skin plasty by local tissues, split auto-dermoplasty, muscle plastic, stem plastic and combined methods.
Published literature about the occurrence of FG for men and women is very limited. It is reported that FG occurs in 1.6 out of 100,000 males annually in the U.S., and most frequently occurs in males 50-79 years (3.3 out of 100,000) (6-8). Between March 2013 to May 2018, 12 cases of FG in patients taking an SGLT2 inhibitor were reported. FG developed within several months of the patients starting an SGLT2 inhibitor. Some patients required multiple disfiguring surgeries, some developed complications, and one patient died. In comparison, only six cases of FG were identified in review of other anti-diabetic drug classes over a period of more than 30 years.
It is thought that any of the SGLT2 inhibitors can be associated with FG. How SGLT2 inhibitors increase the risk of FG is unknown. It is “rare” but it can present in general practice as the use of SGLT2 inhibitors increases.
References:
- Sergey A. Chernyadyev, Marina A. Ufimtseva*, Irina F. Vishnevskaya et al. Fournier’s Gangrene: Literature Review and Clinical Cases. Urol Int. 101(1): 91-97. DOI: 10.1159/000490108
- Bruce Short. Fournier gangrene: an historical reappraisal. Internal Medicine Journal 48 (2018) 1157–1160.
- HIROKI MATSUURA, KAZUKI IWASA, MD. Fournier gangrene. JOURNAL OF MEDICINE VOLUME 85 • NUMBER 9 SEPTEMBER 2018
- Singh A, Ahmed K, Aydin A, Khan MS, Dasgupta P. Fournier’s gangrene. A clinical review. Arch Ital Urol Androl 2016; 88(3):157–164. doi:10.4081/aiua.2016.3.157
- Prohorov AV, author. Furnier’s gangrene. Kazan Med J. 2016;97:256–261
- Sorensen MD, Krieger JN, Rivara FP, Broghammer JA, Klein MB, Mack CD, Wessells H. Fournier’s gangrene: population based epidemiology and outcomes. J Urol 2009;181:2120-6.
- Sorensen MD, Krieger JN, Rivara FP, Klein MB, Wessells H. Fournier’s gangrene: management and mortality predictors in a population based study. J Urol 2009;182:2742
- Sorensen MD, Krieger JN. Fournier’s gangrene: epidemiology and outcomes in the general US population. Urol Int 2016;97:249-59.
