
10th April 2020, Dr Chee L Khoo
It’s amazing how quickly news travel during a pandemic. A bit of information came out a few weeks ago that suggests SARS-CoV-2 enters the body via the angiotensin converting enzyme receptor 2 (ACE2) present in abundance in pulmonary tissues. Initial reports out of Wuhan found that patients with chronic obstructive pulmonary disease (COPD), diabetes and hypertension were at higher risks of getting the infection as well as developing the severe form of Covid-19 if they do get the infection. Someone put 2 and 2 together and thought maybe, because patients with hypertension are likely to be on an angiotensin converting enzyme inhibitor (ACEi) or an angiotensin receptor blocker (ARB) these days, being on ACEi/ARB increase their risk of catching Covid-19 or developing severe complications from it. Is hypertension the problem or is the treatment of hypertension the problem? Is it a problem at all? Should we stop ACEi/ARB in patients during this pandemic?
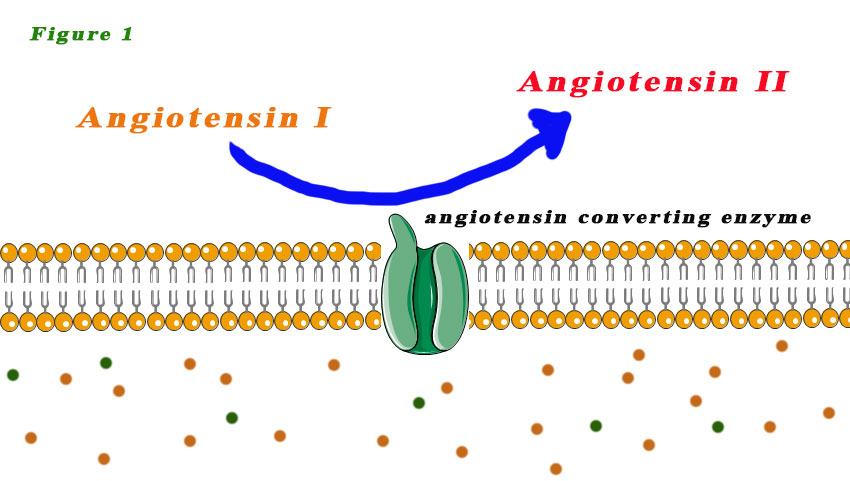
I did touch on the ACE2 receptor last week. It’s worthwhile reviewing them again. We are all familiar with ACE (1) which converts Angiotensin I (ATI) to Angiotensin II (ATII). ATII is a vasoconstrictor which helps keeps our BP up (see Figure 1). Our first line anti-hypertensive these days is often either an ACEi or an ARB which blocks angiotensin converting enzyme (ACE).
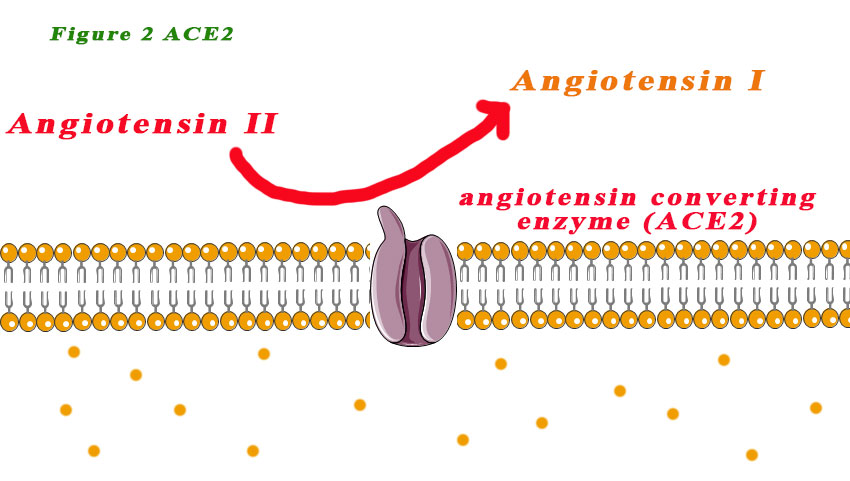
ACE2 was first discovered as a homologue of ACE1 in 2000, which converts angiotensin II to angiotensin 1-7. ACE2 is a type I transmembrane protein, which is mainly anchored at the apical surface of the cell. Its catalytic domain is located at the extracellular side of the cell. It has the opposite effect to the ACE1/ATII system (see Figure 2).
Can ACE inhibitors be harmful?
Losartan and olmesartan have been shown to increase cardiac ACE2 expression about three-fold following chronic treatment (28 days) after myocardial infarction induced by coronary artery ligation of rats (1). Losartan has also been shown to upregulate renal ACE2 expression in chronically treated rats (2). In humans, higher urinary ACE2 levels were observed in hypertensive patients treated with the AT1R antagonist olmesartan (3). These observations suggest that chronic AT1R blockade with ACEi or ARB results in ACE2 upregulation in both rats and humans in cardiac and renal tissues. There are no studies on ACE2 upregulation in pulmonary tissues, though. The significance of elevated serum or urinary ACE2 is unknown.
Because the Covid-19 virus uses the ACE2 receptor as an entry portal, there was concern that this might be why we are seeing a higher risk of Covid-19 in patients with hypertension. Or is it?
Can ACEi be helpful?
ATII not only induce strong vasoconstriction, it also has pro-inflammatory and pro-fibrotic effects. Angiotensin 1-7 on the other hand, induces mild vasodilation as well as anti-proliferative and anti-apoptotic effects. It also has various cardiovascular protective effects, including anti–heart failure, antithrombosis, anti–myocardial hypertrophy, antifibrosis, anti-arrhythmia, anti-atherogensis and attenuating vascular dysfunction related to metabolic syndrome. Essentially, angiotensin 1-7 counterbalance all the “nasty” effects of ATII.
In mice, the SARS-CoV, the SARS virus responsible for the SARS outbreak in 2003, down regulate ACE2 in the lungs leading to worsening of lung injury. The lung injury was improved by treatment with ARB (4). Oudit et al found marked decreased ACE2 expression in the heart of intranasal SARS-CoV–infected mice (5). They also reported that SARS-CoV was isolated from 7 of 20 of the human autopsy hearts, and the myocardial damage was accompanied by the decreased protein expression
of myocardial ACE2 as well. It would appear that SARS-CoV-2 infects the heart and decrease ACE2 receptor expression although direct evidence is still lacking.
A preliminary trial of ACE2 infusion in 10 patients with acute respiratory distress syndrome was completed in humans but was not powered to show efficacy on pulmonary function (6). There is no evidence to demonstrate that treatment with ACEIs or ARBs can decrease severity of pulmonary injury by SARS-CoV-2, though preclinical data suggest a potential mechanism of benefit.
Should patients stop their ACEi or ARB in the context of Covid-19?
The American Heart Association (AHA), the Heart Failure Society of America, and the American College of Cardiology recently put out a joint statement advocating for patients to continue ACEIs and ARBs as prescribed and that changes in medications in the setting of COVID-19 should be completed only after careful assessment (7).
Most research needed
Perhaps, we could analyse clinical patient records and apply data-mining technologies to determine whether patients who were prescribed with AT1R antagonists prior to their diagnosis had better disease outcome. Further, the percentage of people chronically medicated with AT1R
blockers in the general population should be compared with the percentage among hospital admissions of SARS-CoV-2 infected patients presenting with serious symptoms. If the latter percentage would be found to be significantly smaller, this would support the notion that AT1R antagonists confer protection from severe symptoms among SARSCoV-2 infected individuals.
References:
- Ishiyama Y, Gallagher PE, Averill DB, Tallant EA, Brosnihan KB, Ferrario CM. Upregulation of angiotensin-converting enzyme 2 after myocardial infarction by blockade of angiotensin II receptors. Hypertension. 2004;43:970–976.
- Klimas, J., Olvedy, M., Ochodnicka-Mackovicova, K., Kruzliak, P., Cacanyiova, S., Kristek, F., … Ochodnicky, P. (2015). Perinatally administered losartan augments renal ACE2 expression but not cardiac or renal Mas receptor in spontaneously hypertensive rats. Journal of Cellular and Molecular Medicine, 19(8), 1965–1974. https://doi.org/10.1111/jcmm.12573
- Furuhashi, M., Moniwa, N., Mita, T., et al. Urinary angiotensin-converting enzyme 2 in hypertensive patients may be increased by olmesartan, an angiotensin II receptor blocker. American Journal of Hypertension, 28(1), 15–21. https://doi.org/10.1093/ajh/hpu086
- Kuba K, Imai Y, Rao S, et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat Med. 2005;11 (8):875-879. doi:10.1038/nm1267
- Oudit GY, Kassiri Z, Jiang C, Liu PP, Poutanen SM, Penninger JM, Butany J. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Invest. 2009;39:618–625.
- Khan A, Benthin C, Zeno B, et al. A pilot clinical trial of recombinant human angiotensin-converting enzyme 2 in acute respiratory distress syndrome. Crit Care. 2017;21(1):234.
- American Heart Association. HFSA/ACC/AHA statement addresses concerns re: using RAAS antagonists in COVID-19. Accessed April 9, 2020. https://professional.heart.org/professional/ScienceNews/UCM_505836_HFSAACCAHAstatement-addresses-concerns-re-using-RAASantagonists-in-COVID-19.jsp
