18th December 2022, Dr Chee L Khoo
Making a decision whether to treat patients with lipid lowering agents is relatively easy in patients who either have symptomatic cardiovascular (CV) disease or have a very low risk according to our CV risk assessment. It is a bit more difficult in the intermediate CV risk group. We have to consider the cost and adverse effects of initiating lifelong preventive therapy versus the potential benefit to the patient. We also have to consider how aggressive to investigate them. One of the most important CV risk assessment tools is the coronary artery calcium (CAC) score. How good is it in predicting future CV events? How good are you in interpreting the results? When does the patient with zero score need another scan? More importantly, who needs a further CAC score?
What is CAC score?
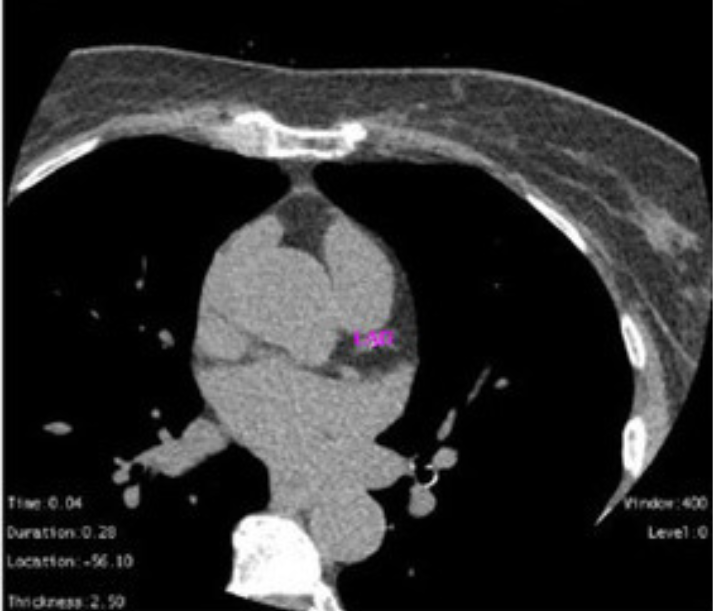
Agatston score is a semi-automated tool to calculate a score based on the extent of coronary artery calcification detected by an unenhanced low-dose CT scan. It was back in 1990 when Agatston et al reported that CAC score was strongly associated with clinical coronary heart disease. They scored CAC in each person as a product of plaque area and peak plaque density, summing across all plaques in each of the 4 coronary arteries, thus upweighting the score when the calcium was more dense. Rather than predicting future events based on the presence or absence of risk factors, CAC measures the actual disease, atherosclerosis, with the probability of a future ASCVD event directly proportional to the degree of CAC.
In the ensuing next 30 years, multiple studies worldwide have demonstrated that CAC measurement methodology is replicable and highly predictive of not only future CHD events but atherosclerotic cardiovascular disease (ASCVD) events more generally.
How do you interpret the results?
Before we can work out how to interpret the results, we need to find out how the “score” is calculated. It is based on weighted density score given to the highest attenuation value (HU) multiplied by the area of the calcification speck. The attenuation value (HU) is given a density factor:
- 130-199 HU: 1
- 200-299 HU: 2
- 300-399 HU: 3
- 400+ HU: 4
For example, if a calcified speck has a maximum attenuation value of 400 HU and occupies 8 sq mm area, then its calcium score will be 32.
The score of every calcified speck is summed up to give the total calcium score. This is the basis of the Agatston score. The result is then categorized into:
- CAC = 0 – Very low risk
- CAC = 1-99 – Mildly increased risk
- CAC = 100-299 – Moderately increased risk and
- CAC > 300 – Moderate to severely increased risk
The Agastston score can also be expressed as a age-, sex-, and race-specific percentile that is derived using the MESA risk score calculator (see below). The absolute score is the best predictor of the total risk of a CHD event for an individual in the near to midterm (in the next 5 to 10 years). In contrast, the percentile score best represents relative risk of CHD event for the individual compared with other individuals of the same age, race, and sex (25). In this way, the percentile score is the better predictor of lifetime risk of developing CHD. While percentile scores are particularly useful in clinical practice for conveying relative and lifetime risk to patients, the absolute score is of more prognostic value and predicts risk better over the traditional 10-year time horizon.
More than just the score alone
CAC has serves us well over the last 30 years and in multiple studies worldwide, this CAC measurement methodology has proved to be replicable and highly predictive of not only future CHD events but atherosclerotic cardiovascular disease (ASCVD) events more generally (1,2) but can we improve on the CAC score?
CAC Score Progression and “warranty period”
Some studies suggest that progression of CAC score over time may better in predicting subsequent CHD events and overall mortality (3,4). The conversion from CAC score of 0 to CAC of greater than 0 over time was found to be nonlinear and dependent on age, sex, and baseline risk profile (5).
This then brings up the question of when to repeat another CAC score if the baseline CAC is 0. This is sometimes referred to the warranty period for which the CAC score of 0 is still valid for the individual. Emerging consensus suggests repeat CAC scans at 5–7 years for individuals with low 10-year CVD risk (< 5% risk), 3–5 years for individuals with intermediate risk (5%–20% risk), and approximately 3 years for individuals with high risk (> 20% risk) or individuals with diabetes mellitus, provided a reassessment will impact clinical management (6,7).
CAC Density and CAC >1000
While CAC scores of greater than 300 or greater than 400 have been traditionally recognized as the highest risk classification of CAC, there are however a unique group of individuals with CAC scores of greater than 1000, many of whom are asymptomatic at the time of scanning. It is thought that in some, the high scores are influenced by high CAC density which may be associated with more stable plaques. However, some individuals with high scores may have high calcified areas as well as extra-coronary calcification. These patients have been found to have as much risk as those in secondary prevention (who have had prior myocardial infarction), suggesting that even more aggressive management of modifiable risk factors might be warranted in this subgroup of individuals.
Criqui et al reported that both CAC volume (positive association) and CAC density (inverse association) gives better prediction if entered separately into the risk model (4,8). This finding is consistent with observations that statins, which are highly protective against CVD, appear to increase the Agatston score (9,10), and very dense (1K) plaque is associated with lower risk (11). Additionally, it has been shown that endurance athletes have higher CAC scores with more calcified plaque and that physical activity in general is tied to faster CAC progression, presumably caused by increased density.
The CAC distribution
You may sometimes come across reports that describe the CAC distribution over the coronary tree. Calcification over multiple vessels are associated with high risk of mortality. Similarly, calcification over the left main coronary artery is also associated with the increased mortality.
Who should have a CAC score?
The Cardiac Society of Australia and NZ (CSANZ) suggests “calcium scoring is appropriate for asymptomatic patients at intermediate Framingham risk, for whom there is strong evidence supporting its ability to improve cardiovascular risk assessment (12)”.
The 2019 AHA/ACC recommended that “for persons at intermediate predicted risk (≥7.5 to <20%) by the PCE or borderline (5 to <7.5%) predicted risk, CACs helps refine risk assessment”. In the new update in 2022, they supported “considering anatomical (including CAC score) or functional imaging for CV risk stratification, shared decision-making, and allocation of preventive therapies which will optimize CV risk factors and affirm healthy lifestyle habits.” This recommendation was for patients with type 2 diabetes (T2D).
The AHA/ACC further added that “CAC measurement is not intended as a “screening” test for all, but rather is a decision aid in select adults to facilitate the clinician-patient risk discussion.” So, many experts are recommending CAC scoring with some qualifications – select patients. So, who are these “select” patients?
Using CAC score in primary care
The MESA risk score was developed using sex-balanced multiple ethnic subgroups in the MESA database for the estimation of 10-year CHD risk. It incorporates traditional risk factors (age, sex, high-density lipoprotein cholesterol, systolic blood pressure, antihypertensive medication use, current smoking status, and diabetes) and CAC, as well as family history of heart attack, body mass index, race and ethnicity, and lipid-lowering medication us.
The MESA risk score calculator is currently available and easily accessible for use on the MESA website with an aim to enhance CHD risk assessment and communication between physicians and their patients. It is accessible here.
At least 25% of patients experiencing nonfatal acute myocardial infarction or sudden death had no previous symptoms. The identification of asymptomatic individuals at greater risk of experiencing future cardiovascular events is fundamental for the implementation of preventive strategies in primary care.
The use of the CAC score is not indicated in high-risk patients because aggressive preventive measures would already be indicated in such patients. In general, patients identified as low CV risk do not need a CAC score although a subgroup of patients deemed low CV risk may need a CAC score. These are patients with diabetes or patients with family history of premature CAD (in a male first-degree relative < 55 years of age or female first-degree relative < 65 years of age). In patients with intermediate CV risk, a CAC score may warrant a discussion on further preventative measures including lipid-lowering therapy.
Can we do better than a CAC score?
The CAC and Data Reporting System (CAC-DRS system) combines the Agatston score and the number of vessels with CAC. It was demonstrated to provide better stratification of risk for CHD, CVD, and all-cause death than the Agatston score alone in a large retrospective clinical cohort of asymptomatic individuals free of baseline cardiovascular disease (13).
References:
- Arad Y, Goodman KJ, Roth M, Newstein D, Guerci AD. Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events: the St. Francis Heart Study. J Am Coll Cardiol. 2005;46:158–165.
- Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345.
- Budoff MJ, Hokanson JE, Nasir K, Shaw LJ, Kinney GL, Chow D, Demoss D, Nuguri V, Nabavi V, Ratakonda R, Berman DS, Raggi P. Progression of coronary artery calcium predicts all-cause mortality. JACC Cardiovasc Imaging. 2010 Dec;3(12):1229-36. doi: 10.1016/j.jcmg.2010.08.018.
- Criqui MH, Denenberg JO, Ix JH, McClelland RL, Wassel CL, Rifkin DE, Carr JJ, Budoff MJ, Allison MA. Calcium density of coronary artery plaque and risk of incident cardiovascular events. JAMA. 2014 Jan 15;311(3):271-8. doi: 10.1001/jama.2013.282535. Erratum in: JAMA. 2015 Apr 7;313(13):1374.
- Min JK, Lin FY, Gidseg DS, Weinsaft JW, Berman DS, Shaw LJ, Rozanski A, Callister TQ. Determinants of coronary calcium conversion among patients with a normal coronary calcium scan: what is the “warranty period” for remaining normal? J Am Coll Cardiol. 2010 Mar 16;55(11):1110-7. doi: 10.1016/j.jacc.2009.08.088.
- Dzaye O, Dardari ZA, Cainzos-Achirica M, Blankstein R, Szklo M, Budoff MJ, Lima JAC, Blumenthal RS, Nasir K, Blaha MJ. Incidence of New Coronary Calcification: Time to Conversion From CAC = 0. J Am Coll Cardiol. 2020 Apr 7;75(13):1610-1613. doi: 10.1016/j.jacc.2020.01.047.
- Newman CB, Blaha MJ, Boord JB, Cariou B, Chait A, Fein HG, Ginsberg HN, Goldberg IJ, Murad MH, Subramanian S, Tannock LR. Lipid Management in Patients with Endocrine Disorders: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2020 Dec 1;105(12):dgaa674. doi: 10.1210/clinem/dgaa674. Erratum in: J Clin Endocrinol Metab. 2021 May 13;106(6):e2465.
- Criqui MH, Knox JB, Denenberg JO, et al.Coronary artery calcium volume and density:potential interactions and overall predictivevalue: the Multi-Ethnic Study of Atheroscle-rosis.JAmCollCardiolImg. 2017;10:845–854. 6
- Osei AD, Mirbolouk M, Berman D, et al. Prognostic value of coronary artery calcium score, area, and density among individuals on statin therapy vs. non-users: the Coronary Artery Calcium Consortium. Atherosclerosis. 2021;316:79–83.
- van Rosendael AR, van den Hoogen IJ, Gianni U, et al. Association of statin treatment with progression of coronary atherosclerotic plaque composition. JAMA Cardiol. 2021;6(11):1257–1266.
- van Rosendael AR, Narula J, Lin FY, et al. Association of high-density calcified 1K plaque with risk of acute coronary syndrome. JAMA Cardiol. 2020;5:282–290.
- Liew G, Chow C, van Pelt N, et al. Cardiac Society of Australia and New Zealand position statement: Coronary artery calcium scoring. Heart Lung Circ 2017;26(12):1239–51. doi: 10.1016/j.hlc.2017.05.13
- Dzaye O, Dudum R, Mirbolouk M, Orimoloye OA, Osei AD, Dardari ZA, Berman DS, Miedema MD, Shaw L, Rozanski A, Holdhoff M, Nasir K, Rumberger JA, Budoff MJ, Al-Mallah MH, Blankstein R, Blaha MJ. Validation of the Coronary Artery Calcium Data and Reporting System (CAC-DRS): Dual importance of CAC score and CAC distribution from the Coronary Artery Calcium (CAC) consortium. J Cardiovasc Comput Tomogr. 2020 Jan-Feb;14(1):12-17. doi: 10.1016/j.jcct.2019.03.011.
