9th December 2023, A/Prof Chee L Khoo
We know how effective statins are in lowering cholesterol levels. Lowering of cholesterol levels, especially LDL-C, have been shown to incrementally reduce adverse cardiovascular events in patients with atherosclerotic disease. We have data to show that for every 1 mmol/L of LDL-C reduction there is a 23% reduction in cardiovascular events, which means, the lower the better (1). This is great because we now have monoclonal antibodies and small interfering RNA agents which can inhibit proprotein convertase subtilisin kexin type 9 (PCSK9). Reducing PCSK9 level reduces LDL-C as they both share receptors in the liver. However, does the addition of PCSK9 inhibitors to statin therapy reduce cardiovascular end points?
ODYSSEY (2)
18,924 patients who had an acute coronary syndrome 1 to 12 months earlier, had an LDL-C level of at least 1.8 mmol/L were randomised to either fortnightly 75mg alirocumab subcutaneously or placebo in addition to high intensity or maximally tolerated statins. The dose of alirocumab was adjusted under blinded conditions to target an LDL-C level of 0.6 to 1.3 mmol/L. After a mean duration of 2.8 years, there was a statistically significant reduction of composite CV end points (coronary heart disease, nonfatal myocardial infarction, fatal or nonfatal ischemic stroke, or unstable angina requiring hospitalisation) of 15%.
FOURIER (3)
27,564 patients with atherosclerotic cardiovascular disease and LDL cholesterol levels of at least 1.8 mmol/L were randomised to either evolocumab 140mg fortnightly or 420mg monthly sci or placebo in addition to high intensity or maximally tolerated statins. After an average of 2.2 years, the mean LDL-C levels were reduced from 2.4 mmol/L to 0.78 mmol/L. The evolocumab group had a 15% reduction in CV end points.
Plaques
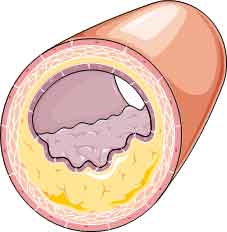
All great results. Yes, reducing LDL-C as expected reduce CV events. What does reduction in LDL-C do to the actual arterial plaques? Our understanding of the composition of arterial plaques and how they cause occlusion has come a long way. It’s not just the size or the volume of the plaque that determines the risk of acute events. The composition of atherosclerotic plaques largely affects their likelihood to progress or trigger acute coronary events (4). Coronary plaques that are prone to rupture or erode and cause adverse cardiac events are characterised by large plaque burden, large lipid content and thin fibrous caps. Intracoronary imaging modalities can evaluate coronary plaque morphology and composition in vivo (5).
We can now assess plaque morphology by intravascular ultrasonography (IVUS), near-infrared spectroscopy (NIRS) or optical coherence tomography (OCT). Large atheroma burden assessed via (IVUS) (6), large lipid burden assessed via (NIRS) (7) and presence of thin fibrous caps assessed via OCT 9 have been associated with a higher risk of subsequent cardiovascular adverse events (8).
Intensive statin therapy has been shown to halt the progression of coronary atheroma burden and might favourably affect plaque composition by reducing plaque lipid content and increasing the thickness of the fibrous cap (9-11).
What can the new PCSK9 inhibiting agents do?
PACMAN-AMI is a double-blind, placebo-controlled trial which enrolled 300 patients undergoing percutaneous coronary intervention for acute myocardial infarction at 9 academic European hospitals (12). Patients who just had an AMI and has undergone urgent PCI on the culprit lesion. Participants were randomised to either 150mg alirocumab fortnightly or placebo. IVUS, NIRS and OCT were serially performed in the 2 non–infarct-related coronary arteries at baseline and after 52 weeks.
IVUS was used to assess percent atheroma volume (lower better). NIRS was used to lipid core burden index within 4mm (lower better). OCT was used to assess fibrous core index (higher better).
After 52 weeks, in comparison with placebo, alirocumab added to high intensity statins, resulted in greater reduction in percent atheroma volume (-2.13% vs -0.92%), greater reduction in maximum lipid core burden index within 4mm (-79.42 vs -37.60) and a greater increase in fibrous core index (62.67 µm vs 33.19 µm). In other words, alirocumab not only reduce the plaque volume but favourably improve the composition of the plaque making it less likely to rupture or erode.
In summary, we now have evidence that “extreme” lowering of LDL-C results in significant plaque regression in the other arteries in patients who just had an AMI. We know from the ODYSSEY and FOURIER trials that addition of a PCSK9 inhibiting agent to high intensity statins reduce cardiovascular events. PACMAN-AMI demonstrated that reduction of LDL-C also change the composition of the lipid filled plaque.
When we have patients discharged from hospital following a cardiovascular event, as GPs, we need to be proactively reducing our patients’ LDL-C below 1.8 mmol/L with what agents we can get our hands on. <1.8 mmol/L is not always achievable with high dose statins +/- ezetimibe. Often, we need to add a PCSK9 inhibitor. With agreement with the treating cardiologist, we can initiate them under the PBS authority. Further reduction of LDL-C below 1.8 mmol/L will reduce the residual risks of cardiovascular events in these patients. Are you complicit in allowing more cardiovascular events to occur in these patients?
References:
- CTT Collaboration. Lancet Vol 376 Nov 13, 2010
- Schwartz G, et al. Alirocumab and Cardiovascular Outcomes after Acute Coronary SyndromeN Engl J Med 2018; 379:2097-2107 DOI: 10.1056/NEJMoa1801174
- Sabatine M, et al. Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease. N Engl J Med 2017;376:1713-22. DOI: 10.1056/NEJMoa1615664
- Libby P. Mechanisms of acute coronary syndromes and their implications for therapy. N Engl J Med. 2013;368(21):2004-2013. doi:10. 1056/NEJMra1216063
- Johnson TW, Räber L, di Mario C, et al. Clinical use of intracoronary imaging: part 2: acute coronary syndromes, ambiguous coronary angiography findings, and guiding interventional decision-making: an expert consensus document of the European Association of Percutaneous Cardiovascular Interventions. Eur Heart J. 2019;40 (31):2566-2584. doi:10.1093/eurheartj/ehz332
- Stone GW, Maehara A, Lansky AJ, et al; PROSPECT Investigators. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011;364(3):226-235. doi:10.1056/NEJMoa1002358
- Waksman R, Di Mario C, Torguson R, et al; LRP Investigators. Identification of patients and plaques vulnerable to future coronary events with near-infrared spectroscopy intravascular ultrasound imaging: a prospective, cohort study. Lancet. 2019;394(10209):1629-1637. doi:10.1016/S0140-6736(19)31794-5
- Prati F, Romagnoli E, Gatto L, et al. Relationship between coronary plaque morphology of the left anterior descending artery and 12 months clinical outcome: the CLIMA study. Eur Heart J. 2020;41(3): 383-391.
- Nicholls SJ, Ballantyne CM, Barter PJ, et al. Effect of two intensive statin regimens on progression of coronary disease. N Engl J Med. 2011; 365(22):2078-2087. doi:10.1056/NEJMoa1110874
- Nissen SE, Nicholls SJ, Sipahi I, et al; ASTEROID Investigators. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis:the ASTEROID trial. JAMA. 2006;295(13):1556-1565. doi:10.1001/jama.295.13.jpc60002
- Kini AS, Baber U, Kovacic JC, et al. Changes in plaque lipid content after short-term intensive versus standard statin therapy: the YELLOW trial (reduction in yellow plaque by aggressive lipid-lowering therapy). J AmColl Cardiol. 2013;62 (1):21-29. doi:10.1016/j.jacc.2013.03.058
- Räber L, Ueki Y, Otsuka T, Losdat S, et al; PACMAN-AMI collaborators. Effect of Alirocumab Added to High-Intensity Statin Therapy on Coronary Atherosclerosis in Patients With Acute Myocardial Infarction: The PACMAN-AMI Randomized Clinical Trial. JAMA. 2022 May 10;327(18):1771-1781. doi: 10.1001/jama.2022.5218. PMID: 35368058; PMCID: PMC8978048.
