10th March 2024, A/Prof Chee L Khoo
Myocardial infarction in a patient with minimal coronary artery disease (stenosis <50%) is increasingly being recognised in patients with myocardial injury but no significant coronary obstruction is demonstrated. Myocardial Infarction in Non-Obstructive Coronary Arteries (MINOCA) accounts for approximately 5-10% of all myocardial infarction. The precise pathogenesis is poorly understood. Diagnosing MINOCA is not straightforward and identifying the aetiologies and ongoing management can be challenging. Compared with traditional MI from coronary artery disease (MI-CAD), the prognosis is only slightly better but it is definitely not benign.
In the past 50 years, the innovation and development of medical technology have allowed us to decipher the aetiologies of MINOCA better. MINOCA is a group of heterogeneous diseases with different mechanisms of pathology. The advent of cardiac MRIs, intravascular US (IVUS) and coronary OCT has allowed better differentiation of the causes of MINOCA and thence, their management.
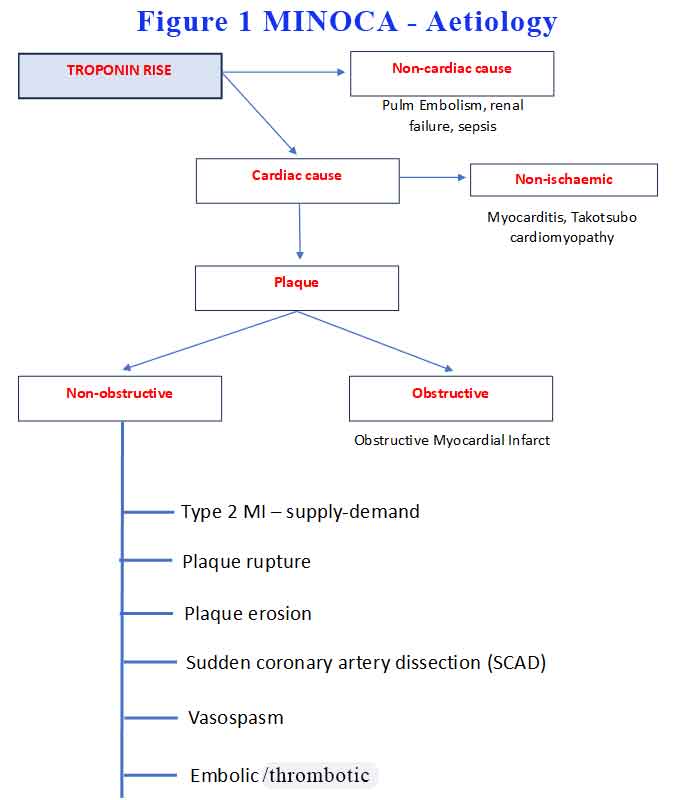
When MINOCA is suspected, a comprehensive search for other causes of troponin rise is conducted. We need to exclude pulmonary embolism, renal failure sepsis, stroke or subarachnoid haemorrhage. When we are confident that the troponin rise is from cardiac causes, we need to decide whether the myocardial damage is ischaemic or non-ischaemic. See Figure 1.
How common is MINOCA?
The recorded prevalence of MINOCA differs according to different approaches to understanding the definition of MINOCA and gathering information. Previous studies demonstrated that the prevalence of MINOCA in patients with AMI is 1–15%. Pasupathy et al. meta-analysed 28 studies and reported that MINOCA occurs in 6% of MI with a female prevalence of 40% diagnosed at a median age of 55 (2). Compared with patients with MI-CAD, MINOCA patients were more likely to be younger (55 vs. 61 years), female (43% vs. 24%), and had less hyperlipidaemia (21% vs. 32%) than obstructive CAD, respectively. Anxiety and depression are also frequent in MINOCA patients relative to MI-CAD and directly related to poor prognosis [3-5].
Prognosis
Comparisons of prognosis of MINOCA and MI-CAD patients are challenging because of the variations in the relevant pathophysiological mechanisms. MINOCA is definitely not benign in its prognosis. In a systematic review, the 12-month all-cause mortality rate of patients with MINOCA was found to be 4.7% [6]. A meta-analysis of MINOCA and MI-CAD clinical manifestations and prognosis showed a high risk for adverse events in patients with MINOCA. The rates of 1-year all-cause mortality, MI, all-cause mortality + MI, cardiac death, and MACE were 2.4, 1.2, 4.0, 1.4, and 9.2%, respectively [7].
The KAMIR-NIH study found that there was no difference between the prognosis of MINOCA and MI-CAD patients in 2 years of follow-up (9.1 and 8.8%, respectively), as well as no significant difference in CV death, noncardiac death, and reinfarction between 2 groups [8]. The COAPT study revealed a 1-year mortality/re-MI rate in MINOCA patients of 5.3% and a 5-year mortality rate of 10.9% (9).
A current study has shown that reduced LV ejection fraction, nonobstructive CAD, ß-blockers during follow-up, and ST depression on ECG at admission are independent predictors of the long-term prognosis of MINOCA patients (10). Another study revealed that female sex, younger age, STE, atrial fibrillation, and a history of previous MI were independent predictors of MINOCA (11). A recent study on prognostic risk factors for MINOCA during a 4.5-year follow-up reported that age, hypertension, diabetes, smoking, previous stroke, MI, peripheral vascular disease, COPD, decreased LV ejection fraction, lower total cholesterol levels, and higher creatinine levels were independent predictors of MACE (12).
Management
Since MINOCA has many possible pathological mechanisms, it is not certain that the classical secondary prevention and treatment strategy for traditional (type 1) MI are suitable for MINOCA patients. Nonetheless, Lindahl et al. showed that MINOCA treatment with statins or ACEI/ARB has a long-term beneficial effect on the outcome, and ß-blocker treatment a positive trend, but that dual anti-platelet therapy (DAPT) has a neutral effect (13). Similarly, The KAMIR-NIH study showed that the use of renin-angiotensin inhibitor blockers (ACEI) and statins for MINOCA patients during a 2-year follow-up was associated with reduced mortality (8).
You would have thought that because this is a coronary event, anti-platelet would reduce MACE. Because of the diverse aetiology and prognosis, the key to the treatment of MINOCA is to identify the etiology. For example Ishii et al. found that in patients with MINOCA, long-term use of aspirin after discharge could not reduce adverse CV events (14). Other studies have shown that intensive clopidogrel therapy tends to be associated with an increased risk of CV mortality, MI, and stroke in MINOCA patients. Thus, antiplatelet treatment is not routinely recommended.
On March 27, 2019, the American Heart Association (AHA) released guidelines for the diagnosis and management of MINOCA [15]; according to the recommendations, risk stratification and the most appropriate treatment scheme should be selected on the basis of aetiology. For MINOCA patients with plaque rupture, DAPT is recommended for 1 year, and single antiplatelet therapy is recommended for life to those suspected of or diagnosed with plaque rupture and MINOCA. If only a mild degree of atherosclerosis is found on coronary angiogram, statins are also recommended. MINOCA caused by coronary spasm can be treated with calcium-channel blocker (CCB) and nitrates.
As you can see MINOCA is a group of heterogeneous diseases arising from a variety of potential causes. Their management obviously depends on the aetiology of MINOCA. While the investigations and management after myocardial injury may not be the concerns of primary care physicians, what about angina arising out of non-obstructive coronary artery disease? These are patients with symptoms of myocardial ischaemia but our standard usual investigations ruled out obstruction as the main cause of the ischaemia. These patients may either undergo further investigations or be reassured that the symptoms are non-cardiac. These are the patients whom we don’t want to miss and they went on to have a MINOCA. We need to listen to our patients and perhaps, refer the patients back to the cardiologist with the question “could this be a MINOCA in the making?”
References:
- Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Circulation. 2018;138(20):e618–51. https:// doi. org/ 10. 1161/ CIR. 00000 00000 000617/ FORMAT/EPUB.
- Pasupathy S, Air T, Dreyer RP, Tavella R, Beltrame JF. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries. Circulation. 2015;131(10):861–870. https:// doi. org/ 10. 1161/ CIRCU LATIO NAHA. 114. 011201/FORMAT/ EPUB.
- Daniel M, Agewall S, Berglund F, Caidahl K, Collste O, Ekenbäck C, et al. Prevalence of Anxiety and Depression Symptoms in Patients with Myocardial Infarction with Non-Obstructive Coronary Arteries. Am J Med. 2018 Sep; 131(9): 1118–24.
- Gu XH, He CJ, Shen L, Han B. Association Between Depression and Outcomes in Chinese Patients with Myocardial Infarction and Nonobstructive Coronary Arteries. J Am Heart Assoc. 2019 Mar; 8(5):e011180.
- Daniel M, Agewall S, Caidahl K, Collste O, Ekenbäck C, Frick M, et al. Effect of Myocardial Infarction with Nonobstructive Coronary Arteries on Physical Capacity and Quality-of-Life. Am J Cardiol. 2017 Aug; 120(3):341–6.
- Pasupathy S, Air T, Dreyer RP, Tavella R, Beltrame JF. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries. Circulation. 2015 Mar; 131(10): 861–70.
- Pizzi C, Xhyheri B, Costa GM, Faustino M, Flacco ME, Gualano MR, et al. Nonobstructive Versus Obstructive Coronary Artery Disease in Acute Coronary Syndrome: A Meta-Analysis. J Am Heart Assoc. 2016 Dec;5(12):e004185.
- Choo EH, Chang K, Lee KY, et al.; KAMIR-NIH Investigators. Prognosis and Predictors of Mortality in Patients Suffering Myocardial Infarction with Non-Obstructive Coronary Arteries. J Am Heart Assoc. 2019 Jul; 8(14):e011990.
- Bainey KR, Welsh RC, Alemayehu W, et al. Population-level incidence and outcomes of myocardial infarction with non-obstructive coronary arteries (MINOCA): insights from the Alberta contemporary acute coronary syndrome patients invasive treatment strategies (COAPT) study. Int J Cardiol. 2018 Aug; 264: 12–7.
- Pelliccia F, Pasceri V, Niccoli G, et al. Predictors of Mortality in Myocardial Infarction and Nonobstructed Coronary Arteries: A Systematic Review and Meta-Regression. Am J Med. 2020 Jan; 133(1): 73–83.e4.
- Montenegro Sá F, Ruivo C, Santos LG, et al. Myocardial infarction with nonobstructive coronary arteries:a single-center retrospective study. Coron Artery Dis. 2018 Sep; 29(6)
- Nordenskjöld AM, Baron T, Eggers KM, Jernberg T, Lindahl B. Predictors of adverse outcome in patients with myocardial infarction with non-obstructive coronary artery (MINOCA) disease. Int J Cardiol. 2018 Jun; 261: 18–23.
- Lindahl B, Baron T, Erlinge D, Hadziosmanovic N, et al. Medical Therapy for Secondary Prevention and Long-Term Outcome in Patients with Myocardial Infarction with Nonobstructive Coronary Artery Disease. Circulation. 2017 Apr;135(16): 1481–9.
- Ishii M, Kaikita K, Sato K, Yamanaga K, Miyazaki T, Akasaka T, et al. Impact of aspirin on the prognosis in patients with coronary spasm without significant atherosclerotic stenosis. Int J Cardiol. 2016 Oct; 220: 328–32.
- Tamis-Holland JE, Jneid H, Reynolds HR, Agewall S, Brilakis ES, Brown TM, et al.; AHA Interventional Cardiovascular Care Committee of the Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; Council on Epidemiology and Prevention; and Council on Quality of Care and Outcomes Research. Contemporary Diagnosis and Management of Patients with Myocardial Infarction in the Absence of Obstructive Coronary Artery Disease: A Scientific Statement from the AHA. Circulation. 2019 Apr; 139(18):e891–908.
