23rd May, 2019. Dr Chee L Khoo
How to implement a low calorie diet for weight loss in general practice
In the last issue, we described our retrospective audit of all the patients at my practice who has a diagnosis of type 2 diabetes and who was offered a low calorie, low carbohydrate diet program between January and May 2018. In general, all patients with type 2 diabetes were offered a partial meal replacement (two sachets plus a meal) and regular follow up over the subsequent 12 months. These include patients who have type 2 diabetes for more than 6 years, patients on insulin therapy and patients with major mental illness.
The following patients were also not offered the diet program:
- Type 1 diabetes
- >75 years old
- <18 years old
- Pregnant
- Major medical co-morbidity e.g liver failure, cancers
- Unable to commit to regular follow up of at least monthly for the first 3 months
- Unable or not prepared to commit to dietary changes
- Normal or underweight (BMI<25 in Caucasians or <23 Asians) who has HbA1c <6.0%
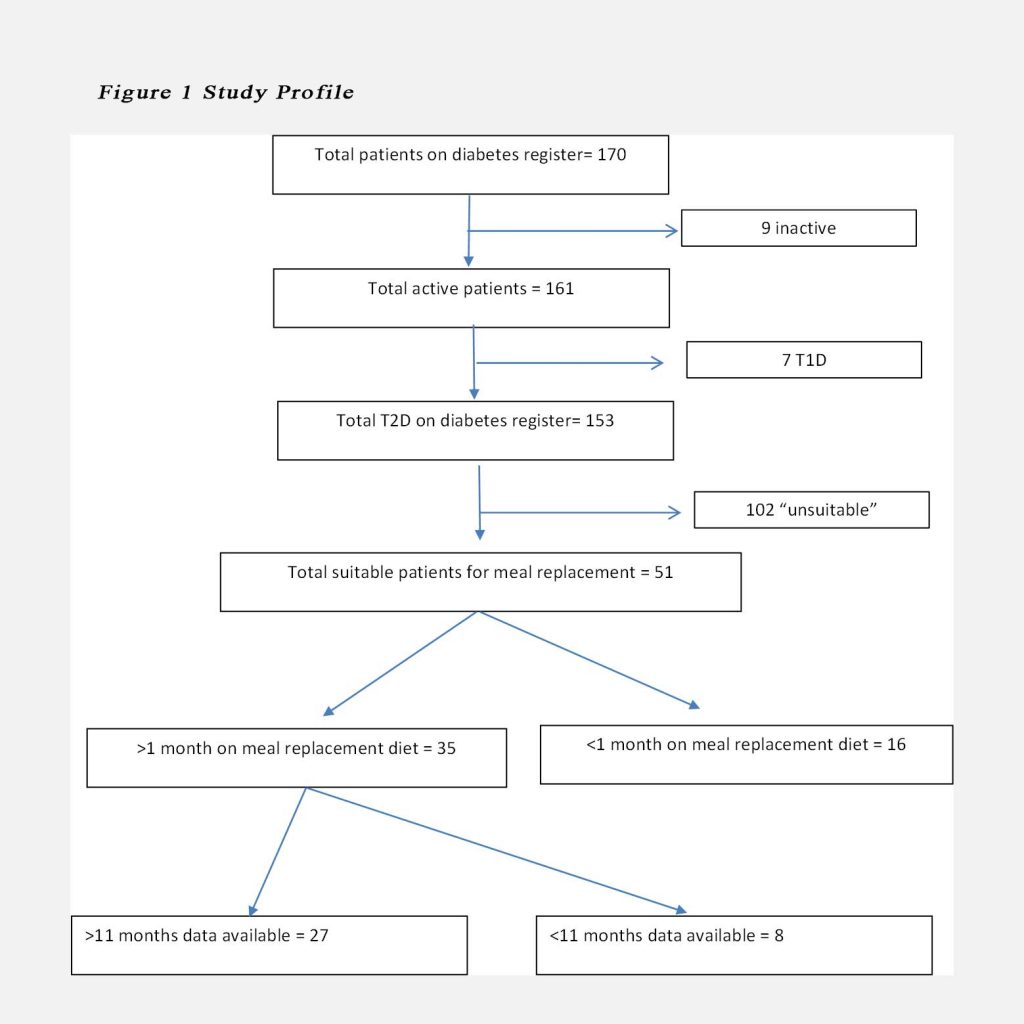
Patients who did not return for the first two months of review were considered not to have completed the partial meal replacement and were not included in the audit (see Figure 1). Not all patients who return for their review at first month persisted with the partial meal replacement beyond the first month. Most patients remained on a lower carbohydrate diet irrespective whether the meal replacement was used.
Data Collection
Weight measures were collected at baseline, 1 month, 2 months, 3 months, 6 months and 12 months. HbA1c, fasting blood glucose levels, lipid profile (total cholesterol, triglycerides, HDL-Cholesterol and LDL-Cholesterol) and eGFR were collected at baseline, 3 months, 6 months and 12 months. Anti-diabetic medications at baseline and at 12 months were recorded. Not all patients return for their scheduled reviews beyond the 1st month. Only patients who have data at 12 months were included in study. There were some patients who started on the meal replacement program after May 2018 and were not included in the study. See Fig. 1
The results
Recruitment and follow up
Overall, there were 170 patients on the diabetes register. After excluding inactive patients, patients with type 1 diabetes, patients that have poor attendance record and patients who were not ready for change, 51 patients accepted the offer of the diet intervention. 16 patients did not follow through with the diet after one month and were not included in the analysis. Of the remaining 35, only 27 had complete data for more than 11 months (see Fig.1).
Table 1. Patient baseline demographics
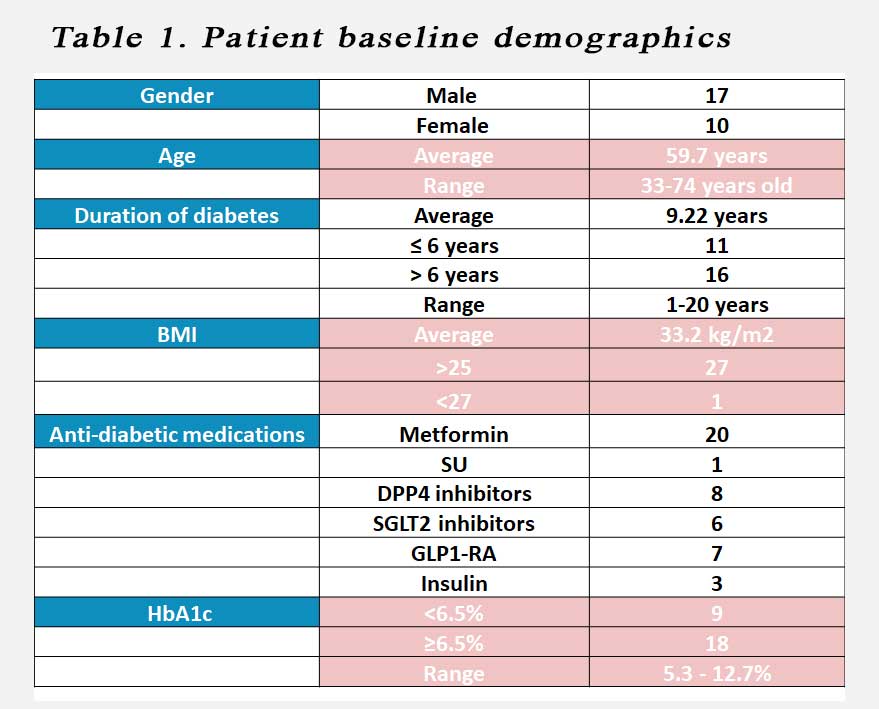
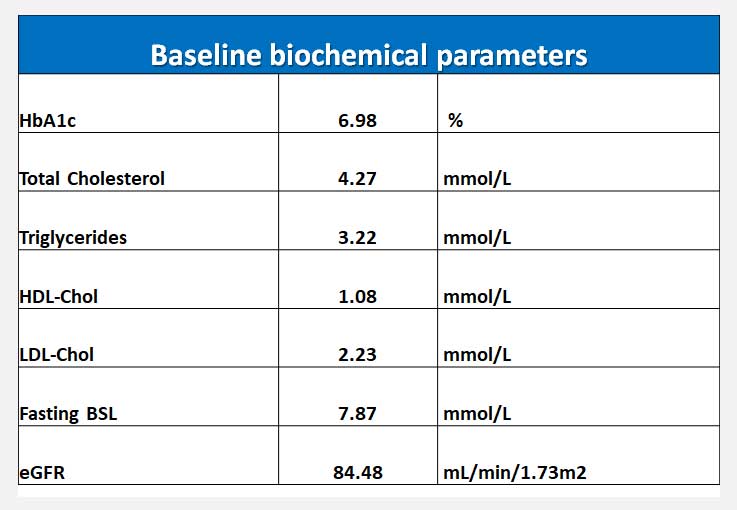 Table 2. Mean baseline biochemical parameters.
Table 2. Mean baseline biochemical parameters.
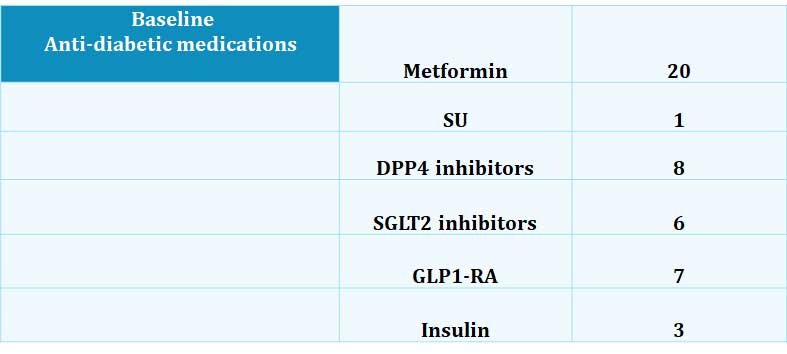
Most patients were on metformin. Only 1 patient was on a sulphonylurea at baseline. This was stopped as the patient commenced on the diet plan. 8 patients were on a DPP4 inhibitors, 6 patients were on an SGLT2 inhibitors while 7 were on a GLP1-RA. Three patients were on basal insulin.
At 12 months, the mean weight lost was 6.25 kg (-6.3±6.4kg, p<0.001). At 12 months, there was significant reduction in weight (-6.3±6.4kg, p<0.001), HbA1c (-0.67±0.93%, p<0.001) and fasting glucose (-1.6±1.59mmol/L, p<0.05). 52% lost >5kgs weight, and 22% reduced HbA1c by >1.0%. Duration of diabetes did not correlate with weight loss or improvement in glycaemia. There were no significant adverse events including major hypoglycaemia.
Table 3. Baseline medications
Weight loss
While the average weight loss was 6.25kg at the end of 12 months, the range of weight change was between +1.6kg and -30.7kg. Only 3 patients did not lose weight at 1 month and these patients failed to lose any weight by 12 months either. 57% of patients lost at least 5kg at 12 months.
HbA1c improvement
Improvement in HbA1c was evident as early as 3 months. 18 patients (67%) of patients recorded a reduction in HbA1c. The proportion of patients who had a lower HbA1c compared to baseline remained at 67%. 1/3 of those recorded an HbA1c reduction of at least 1%.
Other biochemical parameters
Fasting glucose was significantly reduced from an average of 7.9 mmol/L to 6.3 mmol/L by 12 months. HDL-cholesterol was significantly increased from 1.1 mmol/L to 1.2 mmol/L by 12 months. Mean plasma triglycerides reduced from 3.2 mmol/L to 1.8 mmol/L although this was not statistically significant. The LDL-cholesterol increased from a mean of 2.2 mmol/L to 2.4 mmol/L but once again, it was not statistically significant.
There was a marginal improvement in mean eGFR (84.5 – 86.5 ml/min/1.73 m2) which was both not statistically nor clinically significant.
There were no significant adverse effects reported including significant hypoglycaemia or significant hyperglycaemia.
Overall, there was no correlation between duration of diabetes, patient’s age and weight or biochemical changes.
Diabetes remission?
It was difficult to ascertain whether there were significant diabetes remission because 1) many patients already had low HbA1c (within non diabetes range of ≤6.5%) and 2) many were still taking their anti-diabetic medications even though their HbA1c was good. Of the 27 patients with full 12 month data, 18 of them had HbA1c > 6.5% at baseline. At the end of 12 months, 6 of the 18 had HbA1c < 6.5% (non-diabetic levels). All 6 patients were still on their anti-diabetic medications (2 on Metformin alone, 2 on Metformin + DPP4i, 1 on Metformin + SGLT2i, 1 on Metformin + DPP4i + SGLT2i).
Insulin therapy
Three patients were on basal insulin at baseline. 1 patient was able to stop his insulin (20 units to none), 1 half his insulin dose (30 units to 15 units) and one remained on the same dose (28 units).
We are yet to analyse the change in anti-hypertensive medications.
In summary, low to very low calorie diet was tolerable, safe and effective for most primary care patients with type 2 diabetes. There was significant improvement in body weight, HbA1c, fasting glucose and HDL-cholesterol over 12 months.
For details on how you can implement this diet for your patients, email me for details.
