24th February 2024, A/Prof Chee L Khoo
In May 2022, the US Preventative Services Task Force (USPSTF) recommended that we avoid routine aspirin for primary prevention of CVD for anyone at all (1). In particular, for those between 40–59-year-old with a 10-year CVD risk >10%, the decision to initiate aspirin for the primary prevention should be an individual one as the evidence of the net benefit of aspirin use in this group is small. For those > 60 years, the USPSTF specifically recommends against initiating low-dose aspirin for the primary prevention primarily because the bleeding risks exceeds the benefits. In other words, you have to have a pretty good reason to initiate a discussion on aspirin for primary prevention. Is an elevated lipoprotein (a) level a good reason to initiate that discussion? We now have some data supporting the use of aspirin in these patients.
We explored the role aspirin in primary CVD prevention 18 months ago here. Just to recap, the major change in the recommendations from the USPSTF in April 2022 was based primarily on three notable studies:
The ARRIVE study randomised 12546 participants aged >55 years old with multiple risk factors (except diabetes) to either aspirin or placebo (2). The participants’ 10-year CV risk was 17%. Over a median follow up period of 60 months, they found no evidence of cardiovascular benefit and a small statistically significant increase in gastrointestinal bleeding.
In the ASPREE study, 19114 US and Australian participants > 70 years old who did not have cardiovascular disease were randomised to 100mg aspirin or placebo (3). After a median duration of 4.7 years, low dose aspirin in older healthy adults resulted in a significantly higher risk of major haemorrhage (38% increase) and did not result in a significantly lower risk of cardiovascular disease than placebo.
In the ASCEND study, 15480 participants who did not have existing CVD but had diabetes were randomised to receive 100mg aspirin or placebo (4). After a median follow-up of 7.4 years, aspirin use prevented serious vascular events in persons who had diabetes and no evident cardiovascular disease at trial entry (12% reduction, p = 0.01), but it also caused major bleeding events (29% increase, p = 0.003). The absolute benefits were largely counterbalanced by the bleeding hazard.
While ARRIVE and ASPREE showed no benefits with low dose aspirin in patient at high CV risks (average 10-year risk of 17%), ASCEND did show CV benefits. In all three studies, major bleeding risks were significant with low dose aspirin.
What about patients are higher risk of CVD? The Multi-Ethnic Study of Atherosclerosis (MESA) is a medical research study involving more than 6,000 men and women from six communities in the United States. MESA is sponsored by the National Heart Lung and Blood Institute of the National Institutes of Health. In total, 6814 participants were recruited for the first examination. Data are publicly available through MESA upon formal request.
Bhatia H et al obtained data from MESA to look at participants who had lipoprotein a measured and had data on aspirin use and explored the role aspirin in these patients (5). A total of 6632 participants had relevant data for the study. After propensity‐matching aspirin users and nonusers, there were 2183 participants in the matched cohort, 1760 (80.6%) with lipoprotein(a) ≤50 mg/dL, and 423 (19.4%) with lipoprotein(a) >50 mg/dL. Those with lipoprotein(a) >50 mg/dL were more often female and of Black race with greater prevalence of hypertension, statin use, antihypertensive use, and aspirin use. Those with elevated lipoprotein(a) also had higher total cholesterol, low‐density lipoprotein cholesterol, and high‐density lipoprotein cholesterol.
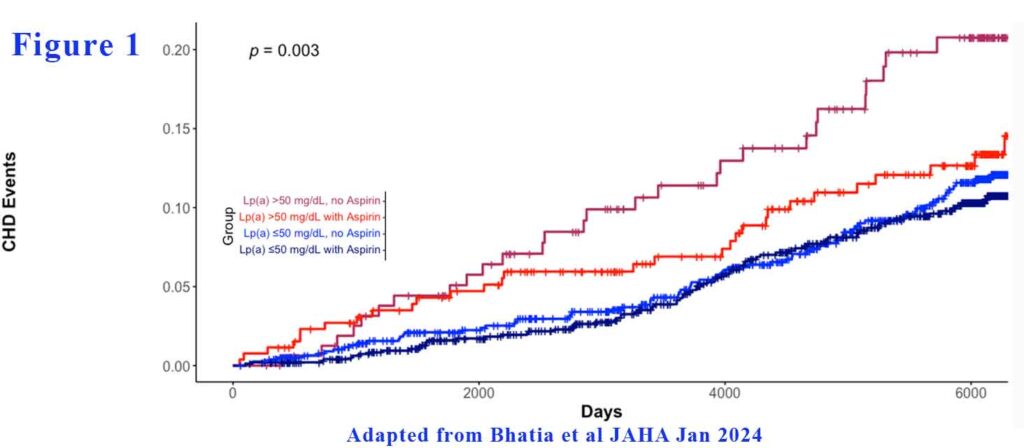
In the propensity‐matched cohort, aspirin use was not significantly associated with a lower risk of CHD events in those with lipoprotein(a) ≤50 mg/dL (hazard ratio [HR], 0.80 [95% CI, 0.58–1.10). However, aspirin use was associated with significantly lower risk of CHD events among those with lipoprotein(a) >50 mg/dL (HR, 0.54 [95% CI, 0.31–0.93]. There were 4 categories of participants: those with elevated Lp (a) not on aspirin, those with elevated Lp (a) on aspirin, those with low Lp (a) not on aspirin and those with low Lp (a) on aspirin. Those with lipoprotein(a) >50 mg/dL without aspirin use had the highest event rate, while those with lipoprotein(a) >50 mg/dL with aspirin use appeared similar to both groups with lipoprotein(a) ≤50 mg/dL (see Figure 1).
Not surprisingly, in the overall cohort, aspirin users were observed to have a higher rate of major bleeding events (n=227, 17.5%) than non-aspirin users (n=655, 12.5%, P<0.001). Among aspirin users, there was no difference in the rate of major bleeding (P=0.224) or the type of bleeding (P=0.070) by lipoprotein(a) level.
At the end of the day, it all comes down to estimating the CV risks in patients who have not had a cardiovascular event (primary prevention). In a 2009 meta‐analysis of primary prevention trials involving aspirin use, aspirin resulted in a 12% relative risk reduction in yearly serious vascular events, but only a 0.07% absolute risk reduction (as compared with a 19% relative risk reduction, and 1.5% absolute risk reduction for secondary prevention).18
The primary prevention definition is becoming a bit murky though. Based on different cardiovascular risk calculators or based on their pre-existing cardiometabolic co-morbidities, many of our patients are at high risk of events. Preventing events in these patients are still considered primary prevention and aspirin is still not recommended. For example, patients with coronary artery stenosis >50% demonstrated on coronary angiogram (invasive or CT) is considered to have established CV disease even if they haven’t had an event. Should they be on aspirin?
This study by Bhatia et al showed that there may be a group that is at high enough cardiovascular risk to derive a benefit from aspirin that outweighs bleeding risk. Given lipoprotein(a)’s interaction with platelets and thrombosis, there is biological plausibility that aspirin may benefit individuals with high lipoprotein(a).
In a secondary analysis of the Women’s Health Study (WHS), which randomized healthy women to aspirin 100 mg every other day or placebo, participants were genotyped for rs3798220, a SNP of the LPA gene (6). Carriers of the rs3798220‐C variant assigned to the placebo group had very elevated lipoprotein(a) levels and significantly elevated CVD risk (HR, 2.24 [95% CI, 1.36–3.68]) compared with noncarriers (6). Carriers who were assigned aspirin had a significant reduction in events (HR, 0.44 [95% CI, 0.20–0.94]) and a similar risk profile as noncarriers assigned aspirin or placebo.
The new Australian CVD Risk Calculator and Multi-Ethnic Study of Atherosclerosis (MESA) calculator comes handy to stratify our patients sitting in front of us. In patients at high or intermediate risk of CVD, aspirin may be warranted. Perhaps, a coronary artery calcium score may assist that discussion further. NIA, Southwest Radiology and Spectrum Medical Imaging all perform a CAC score for between $120-140 as it is not covered by Medicare. A small price for most patients.
References:
- Guirguis-Blake JM, Evans CV, Perdue LA, Bean SI, Senger CA. Aspirin Use to Prevent Cardiovascular Disease and Colorectal Cancer: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2022;327(16):1585–1597. doi:10.1001/jama.2022.3337
- Gaziano JM, Brotons C, Coppolecchia R, et al; ARRIVE Executive Committee. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomised, double-blind, placebo-controlled trial. Lancet. 2018;392(10152):1036-1046. doi:10.1016/S0140-6736(18)31924-X
- McNeil JJ, Wolfe R, Woods RL, et al; ASPREE Investigator Group. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med. 2018;379(16):1509-1518. doi:10.1056/NEJMoa1805819
- Bowman L, Mafham M, Wallendszus K, et al; ASCEND Study Collaborative Group. Effects of aspirin for primary prevention in persons with diabetes mellitus. N Engl J Med. 2018;379(16):1529-1539. doi:10.1056/NEJMoa1804988
- Bhatia HS, Trainor P, Carlisle S, Tsai MY, Criqui MH, DeFilippis A, Tsimikas S. Aspirin and Cardiovascular Risk in Individuals With Elevated Lipoprotein(a): The Multi-Ethnic Study of Atherosclerosis. J Am Heart Assoc. 2024 Feb 6;13(3):e033562. doi: 10.1161/JAHA.123.033562. Epub 2024 Jan 31. PMID: 38293935.
- Chasman DI, Shiffman D, Zee RY, Louie JZ, Luke MM, Rowland CM, Catanese JJ, Buring JE, Devlin JJ, Ridker PM. Polymorphism in the apolipoprotein(a) gene, plasma Lipoprotein(a), cardiovascular disease, and low‐dose aspirin therapy. Atherosclerosis. 2009; 203:371–376. doi: 10.1016/j.atherosclerosis.2008.07.019
